Disclosure of Conflicts of Interest: We certify that all our affiliations with or financial involvement in, within the past 5 years and foreseeable future , any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript are completely disclosed.
Abstract
Department of Pharmacy in Chia Nan University of Pharmacy and Science as the core leader, Tainan Municipal Hospital, Sin-lau Hospital and Kaohsiung branch in Chang Gung Memorial Hospital combined with a complete service network of Community pharmacists work together to improve drug safety as team care.This project enrolled 66 cases, including 38 cases from Kaohsiung branch in Chang Gung Memorial Hospital, 14 cases from Tainan Municipal Hospital, 14 cases from Sin-lau Hospital. The average age of cases was 67.32 ± 13.02 (mean ± s.d.) so that our cases were most elders. We totally enrolled 17 Pharmacists in average 3.9 patients per pharmacist. Before 2010 September, 58 cases were scheduled in our services at least 6 months.
10.83% of drug cost and 23.15% of medical expenditures were found. Meanwhile, the visiting numbers dropped down to 29.67%. Overall, the frequent attendances were decreased. Based on English Drug Code, ACT, 9.49 kinds of drugs were used before our intervention but it was changed by 20% of decrease after our intervention. After analysis of targets personalities, the pre- and post-tests of the collected 38 cases were found that 78.8% of cases feared death (p = 0.008) accompanied by a 91.2% low satisfaction toward their doctors (p = 0.007). At the same time, patients’ satisfaction with this service was also reducing , which means pharmacists made pressure to their visiting targets due to time limitation (p = 0.001). Through this research, targets’ awareness of the health risks occurred from frequent consults (p = 0.002) and the cost effectiveness (p = 0.001) were significantly increased. The most important thing was that our intervention did a great effect on typical frequent attenders 93% (p = 0.003) that means this study has reached its original purposes.
Key words: Pharmacy home-care, Pharmacy service network, Frequent-medicine-use patients, drug and medical expenditures
Introduction
Patients who visit the doctor often, sometimes called“frequent attenders,”1 are common in primary care clinics. Although increased health care use is at times warranted, persistent overuse can have unfortunate consequences for the patient and the medical system. Frequent attenders can suffer through excessive investigations, over treatment, and inappropriate reassurance by the provider . At the same time, frequent attenders exhaust significant resources and put stress on clinic staff. Frequent attenders (FAs) generate a large proportion of general practitioners (GPs)’ clinical workload1. Very frequent attenders account also for a great proportion of GPs’ referrals and prescriptions2. Two systematic reviews show that FAs have high rates of physical disease,emotional distress, psychiatric illness and social difficulties3-11. A systematic review of interventions on FAs found all the interventions in reducing healthcare utilization by FAs to be ineffective5. The interventions analysed were made for the patients who were FAs for up to two consecutive years5. Some 7-33% of FAs persist as FAs in follow-ups6-13. Compared with temporary FAs, persistent FAs consume even more healthcare services and are not diagnosed only with somatic diseases but in particular more social problems, psychiatric problems, and medically unexplained physical symptoms14-25.
Primary hypothesis
Frequent attenders (FAs) generate a large proportion of GPs’ clinical workload. Very frequent attenders account also for a great proportion of GPs’ referrals and prescriptions. The aim of this study will be to examine risk factors that predict persistent healthcare frequent attendance among a frequent attendant (FA) population.
The two-group pre-post design which can be depicted as:

There are two lines in the design indicating that the study is comprised of two groups. The two groups will be non-randomly assigned as indicated by the "N". Both groups including the Burst and Gap's group and the Regular group will be measured before the program occurred as indicated by the first "O" in each line. Following this pre-observation, the group in the first line will be received a program or treatment while the group in the second line will not. Finally, both groups will be measured subsequent to the program.
Materials and Methods
This project enrolled 66 cases, including 38 cases from Kaohsiung branch in Chang Gung Memorial Hospital, 14 cases from Tainan Municipal Hospital, 14 cases from Sin-lau Hospital. The average age of cases was 67.32 ± 13.02 (mean ± s.d.) so that our cases were most elders. We totally enrolled 17 Pharmacists in average 3.9 patients per pharmacist. Before 2010 September, 58 cases were scheduled in our services at least 6 months. Using the Wilcoxon rank-sum test in STATA 10.1 to compare the sixth month of drug expenditures after pharmacists intervention.Before 2010 September, these cases were scheduled in our services at least 6 months (Figure 1).
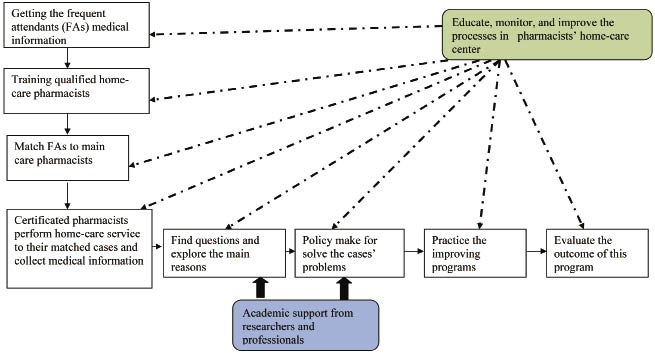
Figure 1. Study frame
Our inclusion criteria are as follows
1. Informed Consent Form assigned.
2. Females or males over 20 years with chronic diseases, such as heart disease, stroke, cancer, chronic respiratory diseases and diabetes, are by far the leading cause of mortality in the world, representing 60% of all deaths.
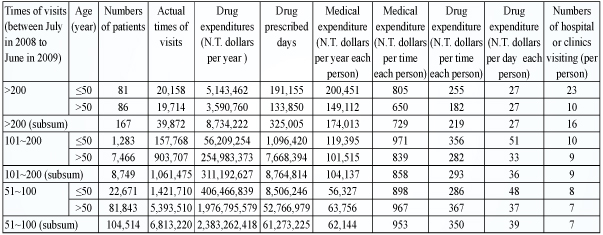
3. Patients had attendance in clinics or hospitals over 50 times between July in 2008 to June in 2009 based on data of National Taiwan Health Insurance,excluding visits in Department of Chinese Medicine, Rehabilitation, Emergency, Dentistry, and Psychosomatics (Table 1).
Table 1.Frequent attendance data in clinics or hospitals from Kao-Ping Branch of National Taiwan Health Insurance between July in 2008 to June in 2009.
Exclusion criteria
1. Patients had died or left the practice since the original consultation data were collected.
2. Patients had a terminal illness or had severe mental illness or impairment.
3. Patients had a severe alcohol or drug problem.
4. Patients had severe sensory impairment.
5. Patients were antisocial, violent, or aggressive; and felt they should not be interviewed (with reason).
6. Dialysis patients.
Pharmacists’ home visiting program to change the Burst and Gap’s (experimental groups) behavior was significantly effective by reducing their medical use in a month than Regular group (control groups). Potential responders were identified by analysis of ‘questionnaires’ ; each individual was classified into two groups:
(1) ‘Regular’ frequent attenders: At least one consultation in every 90-day period, and no periods of 10 consultations over 90 days (a‘burst’);
(2) ‘Burst/gap’ frequent attenders: At least one burst (over 10 consultations in 90 days), and at least one period of no consultations over 90 days (a ‘gap’).
The pharmacists’ home care should be at least six times a year to find out what’s their risk factors inducing their frequent attendance. Frequent attenders generate a large proportion of general practitioners (GPs) clinical workload.
(3) predicting persistent frequent attendance, distinction between temporary and persistent frequent attendance should be drawn.
(4) Persistent frequent attendance in contrast to temporary frequent attendance was related to high body mass index, alcohol abstinence, irritable bowel syndrome, low patient satisfaction, and fear of death.
(5) Bayesian prediction tools are useful for screening risk factors for frequent attendance. Besides, pharmacists’ home-care visiting measured by feedback of evaluation and management note is as our main variables.
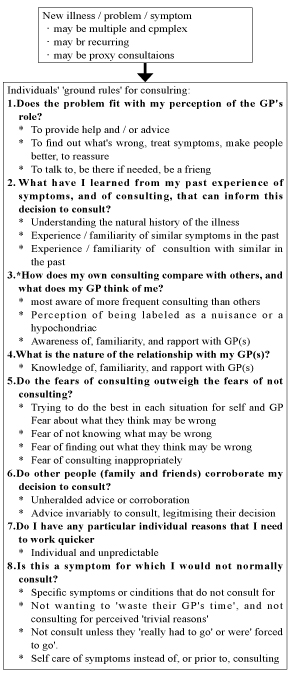
Besides, our dependent variables should be from the NHI data including patients’ demographics, disease diagnosis, contracted medical care institutions, medical expenditure, and prescription claims data. For each medical expenditure reimbursement (both outpatient and inpatient), the types of medical services, details of medical orders, and costs are recorded. The association between the Burst and Gap and risk of frequent attendance was estimated by questionnaire (Appendix A).
Results
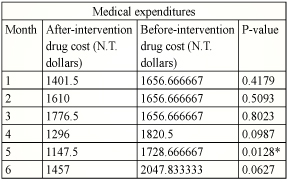
Using the Wilcoxon rank-sum test in STATA 10.1 to compare the sixth month of drug expenditures after pharmacists intervention , 10.83% of drug cost and 23.15% of medical expenditures were found. Meanwhile, the visiting numbers dropped down to 29.67%. Overall, the frequent attendances were decreased. Based on English Drug Code, ACT, 9.49 kinds of drugs were used before our intervention but it was changed by 20% of decrease after our intervention. In comparison of 3-month after-launch and 6-month after-launch, pharmacists’ intervention had made decrease of drug and medical expenditures in half cases. Using Wilcoxon rank- sum test in STATA 10.1 for accounting the monthly costs showed that medical costs in the fifth and sixth months after the intervention (0.0217) was less than one of three months before this intervention (0.0491). Besides, according to the report from National Health Insurance, we found that there was an obvious reducing of drug expenditure (0.0128) in the fifth month of after-launch. Meanwhile, attendances were also 29.67% decrease after the intervention. In Table 2, the medical expenditures were significantly decreasing from N.T. 2977 dollars to 2313 dollars in the 5th month and N.T. 3097 dollars to 2477 dollars in the 6th month. Besides, Drug expenditures also had similar situation in the 5th month in Table 3. Overall, the situation of frequent attendances was improved continuingly.
Table 2. Medical expenditures
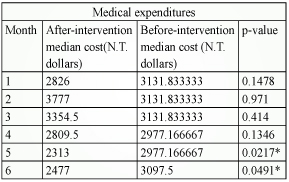
P-value less than 0.05 is significant.
Table 3. Drug expenditures
P-value less than 0.05 is significant.
This study enrolled a total of 52 (22 males and 30 females medical workers) questionnaires, which 28 people (52.8%) less than 40 years, and their occupations were five doctors, 35 pharmacists, a researcher, 10 pharmacy students and a manager in hospital. The results showed that characteristics of pharmacists and pharmacy students tend to have higher positive (p = 0.001) and well-cultured (p = 0.003) personalities. Except hospital manager, physicians (odds ratio odds ratio (OR) 3.32, 95% Confidence level (95% CI) 1.95-7.21, p <0.001), pharmacists (OR 5.67, 95% CI 3.35-9.71, p <0.001), medicine students (OR 3.58, 95% CI 2.83-7.01, p <0.001) and researchers (OR 5.44, 95% CI 3.18-10.55, p = 0.002) all agreed that computer technology could do a great favor in pharmacy network.
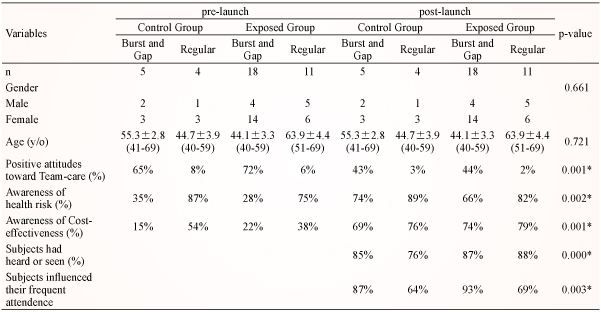
Overall, the various five medical workers showed their positive responses toward this intervention, especially for physicians, pharmacists, and pharmacy students (p = 0.033). After analysis of targets’personalities, the collected 38 cases were divided into two groups by definition of socipsychological theory, Burst and Gap (typical hospital shopper) and Regular (frequent attenders based on their medical needs). We also found that more than 4 chronic diseases (p = 0.002), education level without college (p = 0.001), former frequent attenders (94.6%, p = 0.033) were high-risk factors belonged to Burst and Gap. In particular, 78.8% of cases feared death (p = 0.008) accompanied by a 91.2% low satisfaction toward their doctors (p = 0.007). In pre-tests and post-tests, the control group defined as visiting care less or equal to two times and exposed group defined as visiting care performed per month at least two times, we found that Burst and Gap patients’ satisfaction with this service was reducing from 72% to 44%, which means pharmacists made pressure to their visiting targets due to time limitation (p = 0.001). However, through this research, targets’ awareness of the health risks occurred from frequent consults (p = 0.002) and the cost effectiveness (p = 0.001) were significantly increased. The most important thing was that our intervention did a great effect on typical frequent attenders 93% (p = 0.003) that means Burst and Gap had changed their hospital shopping completely and this study has reached its original purposes (Table 4).
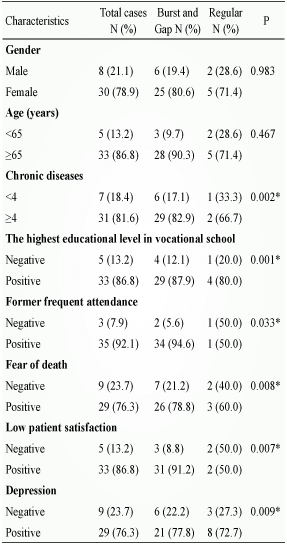
Table 4. Pretest and postest
We found six obvious situations like Table 5. Study patients were a selected group of patients regarding age, chronic diseases, and education. Some 71% of the all study patients had at least four chronic diseases, 67% were aged between 50 and 64 and 84% had the highest educational level in vocational school. A total of 31% of study patients were classified as persistent FAs. We found that the seven most influential predictive risk factors for persistent frequent attendance among FAs were female gender (p=0.001), former frequent attendance (p=0.028), fear of death (p=0.000), multiple chronic diseases (p=0.004), low patient satisfaction and depression (p=0.001).
Conclusions
Overall, Pharmacists’ home visiting program to change the Burst and Gap’s behavior was significantly effective by reducing their medical use in a month than Regular group in one and half months by survival analysis. Generally, Pharmacists’ home care had shown their specificity and effectiveness on typical cases.
Table 5. Characteristics of cases
References :
1. Neal RD, Heywood PL, Morley S, Clayden AD, Dowell AC. Frequency of patients' consulting in general practice and workload generated by frequent attenders: Comparisons between practices. Br J Gen Pract 1998; 48: 895-8.
2. Heywood PL, Blackie GC, Cameron IH, Dowell AC. An assessment of the attributes of frequent attenders to general practice. Fam Pract 1998; 15: 198- 204.
3. Vedsted P, Christensen MB. Frequent attenders in general practice care: A literature review with special reference to methodological considerations. Public Health 2005;119:118-37.
4. Gill D, Sharpe M. Frequent consulters in general practice: A systematic review of studies of prevalence, associations and outcome. J Psychosom Res 1999; 47: 115-30.
5. Smits FT, Wittkampf KA, Schene AH, Bindels PJ, Van Weert HC. Interventions on frequent attenders in primary care: A systematic literature review. Scand J Prim Health Care 2008; 26: 111-16.
6. Andersson SO, Lynoe N, Hallgren CG, Nilsson M. Is frequent attendance a persistent characteristic of a patient? Repeat studies of attendance pattern at the family practitioner. Scand J Prim Health Care 2004; 22: 91-4.
7. Carney TA, Guy S, Jeffrey G. Frequent attenders in general practice: A retrospective 20-year follow-up study. Br J Gen Pract 2001; 51: 567-9.
8. Gill D, Dawes M, Sharpe M, Mayou R. GP frequent consulters: Their prevalence, natural history, and contribution to rising workload. Br J Gen Pract 1998; 48: 1856-7.
9. Semmence A. Chronic high users in a general practice: A preliminary study. J R Coll Gen Pract 1969; 17: 304-10.
10. Vedsted P, Olesen F. Frequent attenders in out-of-hours general practice care: Attendance prognosis. Fam Pract 1999; 16: 283-8.
11. Vrca Botica M, Kovacic L, Kujundzic Tiljak M, Katic M, Botica I, Rapic M, et al. Frequent attenders in family practice in Croatia: Retrospective study. Croat Med J 2004; 45: 620-4.
12. Ward AM, Underwood P, Fatovich B, Wood A. Stability of attendance in general practice. Fam Pract 1994; 11: 431-7.
13. Smits FT, Brouwer HJ, van Weert HC, Schene AH, ter Riet G. Predictability of persistent frequent attendance: A historic 3-year cohort study. Br J Gen Pract 2009; 59: 44-50.
14. Smits FT, Brouwer HJ, ter Riet G, van Weert HC. Epidemiology of frequent attenders: A 3-year historic cohort study comparing attendance, morbidity and prescriptions of one year and persistent frequent attenders. BMC Public Health 2009; 9: 36.
15. Beck AT, Steer RA. Internal consistencies of the original and revised Beck Depression Inventory J Clin Psychol 1984; 40: 1365-7.
16. Antonovsky A. The structure and properties of the sense of coherence scale. Soc Sci Med 1993; 36: 725-33.
17. Sintonen H. The 15D instrument of health- related quality of life: Properties and applications. Ann Med 2001; 33: 328-36.
18. Taylor GJ, Bagby RM, Parker JD. The 20-item Toronto Alexithymia Scale, IV: Reliability and factorial validity in different languages and cultures. J Psychosom Res 2003; 55: 277-83.
19. Derogatis LR, Lipman RS, Covi L. SCL-90: An outpatient psychiatric rating scale: Preliminary report. Psychopharmacol Bull 1973; 9: 13-28.
20. Speckens AE, Spinhoven P, Sloekers PP, Bolk JH, van Hemert AM. A validation study of the Whitely Index, the Illness Attitude Scales, and the Somatosensory Amplification Scale in general medical and general practice patients. J Psychosom Res 1996; 40: 95-104.
21. Raivio R, Jaaskelainen J, Holmberg-Marttila D, Mattila K. Potilastyytyv ä isyyden mittaaminen perusterveydenhuollossa Assessment of patient satisfaction in primary health care: Reliable information and benchmarking]. Suom L ä ä k ä ril 2008; 63: 2622-6 [in Finnish]. English summary.
22. Hauge R, Irgens-Jensen O. Scandinavian drinking journey: Sampling operations and data collections. Oslo: SIFA (National Institute for Alcohol Research); 1981.
23. Ng AY, Jordan MI. Discriminative vs. generative classifi ers: A comparison of logistic regression and naive Bayes. Advances in Neural Information Processing Systems 14. Cambridge, MA: MIT Press; 2002.
24. Soini EJ, Rissanen T, Tiihonen J, Hodgins S, Eronen M, Ryyn ä nen OP. Predicting forensic admissions among the mentally ill in a multinational setting: A Bayesian modelling approach. Data Knowl Engin 2009; 68: 1427-40.
25. Lucas P. Bayesian analysis, pattern analysis, and data mining in health care. Curr Opin Crit Care 2004; 10: 399-403.
摘要
以嘉南藥理科技大學藥學系為中心,與台南市立醫院、新樓醫院及高雄長庚醫院醫療團隊暨社區藥事人員共同建構完善藥事服務網,增進用藥安全。本計畫共收案66名個案,其中38名個案來自高雄長庚醫院,14名個案來自台南市立醫院、14名個案來自新樓醫院。個案的平均年齡為:67.32±13.02,個案年紀偏向中高齡個案。由17位藥師負責照護,平均每位藥師照護3.9位個案。而到99年9月之前,已經有58位個案進入訪視第6個月。藥師介入後的第六個月藥費降低10.83%;醫療總費用則減低23.15%。同時,個案的就診次數與輔導前比較也降低了29.67%,整體次數的趨勢觀察,可發現就診次數呈現持續降低。且在用藥數量的改變以 ACT 藥品英文代碼前7碼為計算基準,介入前平均每個個案使用了9.49樣藥品,但是介入後,用藥品項已下降超過20%。經過人格特質分析,將所收集到38位之有效高診次訪視民眾前後測結果發現,在典型高診次個案裡有高達78.8%害怕死亡 (p=0.008),伴隨著91.2%對看診醫師滿意度低 (p=0.007) 導致了高診次產生;同時發現典型高診次病人中每月訪視的滿意度有下降趨勢,顯示訪視藥師可能因研究時間較短需在短時間達到成效,而造成訪視對象壓力 (p=0.001)。但經由這次計畫,個案意識到高診次對於其健康危害 (p=0.002) 與造成醫療資源成本浪費認知 (p=0.001) 有顯著性提高,最重要的是典型高診次個案因此計畫而改變其醫療行為高93% (p=0.003),顯示本計畫有達成其研究目的。
誌謝
本研究報告由行政院衛生署中央健康保險局所支持〈grant no.DOH99-NH-1006〉,謹此致謝。
作者
嘉南藥理科技大學藥學系副教授 王四切
彰化漢銘醫院藥劑科藥師 許斐凱
台南市立醫院副院長 陳怡
高雄長庚紀念醫院藥劑部藥師 李炳鈺
台南新樓醫院藥劑科藥師 蔡佩瑜