Abstract
Gynecomastia and galactorrhea are two unique adverse effects on breast. Many drugs have been implicated in their cause. We report one case of each condition.
The first case is a 34-year-old woman who reported milk-like discharge from the nipples and irregular menstrual cycle after she had taken mosapride, lansoprazole and sulpiride for 3 months because of gastro-esophageal reflux disorder. She visited our breast-surgery clinic where laboratory tests showed elevated prolactin level 84.00 ng/mL (normal range (NR) level: 5.8-26.53 ng/dL). However, she denied any endocrinology history but drug-related galactorrhea was highly suspected. Sulpiride and lansoprazole were discontinued immediately. The patient's prolactin level was rechecked a month later and showed 12.02 ng/mL within normal range.
The second case is a 61-year-old male who reported bilateral breast enlargement with nipple tenderness following treatment with captopril (12.5 mg twice daily for 2 years and titrated to 25 mg twice daily for 1 month). Laboratory tests of liver transaminases, testosterone and estradiol were within normal limits. Captopril was then discontinued and the symptom disappeared in about one week. One year later, the symptom reoccurred after the patient had taken sulpiride 50 mg twice daily for treatment of abdominal discomfort for 2 months. The symptom also subsided after the patient has discontinued sulpiride.
These two adverse reactions are reversible and these two cases clearly demonstrate that the side effects have disappeared after the patient has discontinued the causative agents. Switching to other alternative agents is the best choice to quit the side effect. Furthermore, a thorough review of medication history will also be helpful to identify the drug adverse reactions.
Keywords: drug adverse reaction, gynecomastia, galactorrhea
Introduction
Various medications have been reported which could potentially induce breast abnormality. In male population, the abnormality was defined as gynecomastia, a benign enlargement of the male breast tissue. In women it was identified as galactorrhea, and it is usually characterized with milk secretion from the breast. This milk secretion is not caused by pregnancy or breast-feeding, but it is mostly complicated by hyperprolactinemia. Hyperprolactinemia is in fact more frequent in women than men. Sometimes it is asymptomatic, the higher the serum prolactin level, the more patients have clinical manifestations. The manifestations include sexual dysfunction, infertility, amenorrhea, gynecomastia or galactorrhea. In gynecomastia, symptoms present like breast pain, swelling, but hormone serum level is normal. Drug induced breast abnormality is a non-physiological event; discontinuation of the offending agents is the most appropriate management. The symptoms will halt which could range from weeks to years. Some severe events may need internal treatment or surgical therapy. In this article, we report one case of each adverse event and reviewed the physiology causes that may lead to both conditions.
一、Medication-induced women breast abnormality
Case presentation
A 34 years old woman who has a 7 years old son, she is either not pregnant or breast-feeding. She was treated with mosapride, lansoprazole, sulpiride for gastro-esphageal reflux disorder in 2012. Her medication record is shown on Table 1. The maintenance treatment should be followed for 3 months.
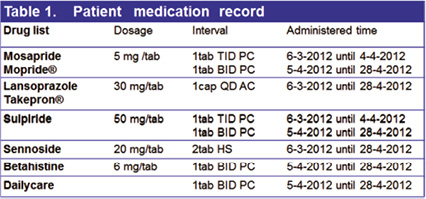
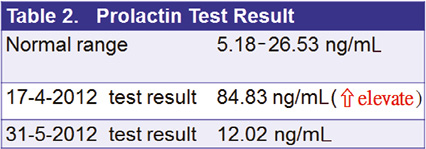
After the first month of treatment, she discovered milk-like discharge from the nipple and irregular menstrual cycle. She visited our breast-surgery OPD and laboratory tests showed the prolactin level rose to 84 ng/mL (normal < 20.0 ng/mL)(Table2).
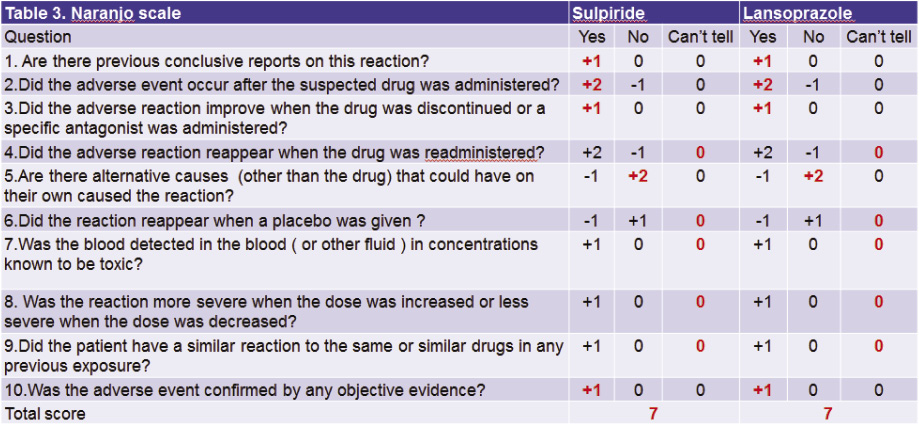
Clinical evaluation including history, physical examination and Naranjo score of drug adverse effect showed 7 which lead it to a probability of medication induced (Table 3).
The clinician recommended terminating sulpiride1 and lansoprazole2,3 used. Two weeks later, the milk-like discharge was gradually reduced. On May, 31st 2012, patient rechecked her prolactin level, it was clearly down to 12.02 ng/mL.
Discussion and management objectives
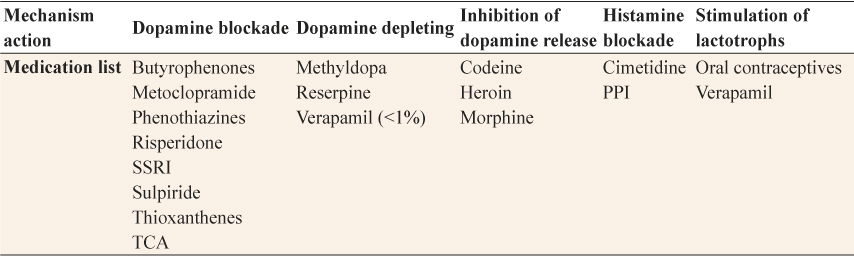
Galactorrhea was defined as a milk-like secretion from the breast in the absence of parturition or beyond 6 months postpartum in a non-breast-feeding woman. This condition is normal in women who are 20-35 years old and in previously parous women and in infants or teenager girls. It is abnormal to be found in children, men and nulligravid women. The abnormal condition can signify a serious underlying disorder that may result in patient anxiety and physician concern. Pharmacologic agents are a common cause of galactorrhea, especially after infancy. Medications associated with galactorrhea are listed in Table 4. The pathophysiology mechanism known to cause galactorrhea are these agents can block dopamine and histamine receptors, deplete dopamine stores, inhibit dopamine release, and stimulate lactotrophs.
Table 4 - Medications associated with galactorrhea
In pharmacologic induced galactorrhea cases, hyperprolactinemia may be indicated. Prolactin level is labile and episodic, it is suggested prolactin level should be confirmed on at least 2 occasions, to determine whether it was pharmacologic induced or likelihood of finding a prolactin-secreting pituitary tumor. There is a direct correlation between the degree of hyperprolactinemia and prolactin-secreting pituitary tumor, therefore when a serum prolactin level indicates greater than 200 ng/mL, it is virtually assure the presence of prolactinoma4,5.
Besides high serum prolactin, symptoms will reveal as a milk-like secretion from the unilateral or bilateral breast. The milky secretion could be intermittent or persistent, scant or abundant, free-flowing or expressible5.
The decision to treat drug induced galactorrhea should be based on the serum prolactin level and severity of galactorrhea and patient's fertility desires. Replaced with safer alternative agents or cease the causative agents are strongly recommended. For most patients with hyperprolactinemia disorder, dopamine agonists are extremely effective in lowering the prolactin level. Bromocriptine and carbegoline are 2 agents approved by U.S FDA for the treatment of hyperprolactinemia.
二、 Medication induced men breast abnormality
Case presentation
A 61years old male patient with history of coronary artherosclerosis, myocardial infarction post percutaneous transluminal coronary angioplasty (PTCA) and hyperlipidemia, had visited the endocrinologist for evaluation of his bilateral breast enlargement with painful on nipple on June 2007. He had taken captopril 12.5 mg twice daily since January 2005, dosage changed to 25 mg twice daily for unstable ischemic events in May 2007. His medications record is listed as following: Isosorbide-5-mononitrate 20 mg 1 tab BID, Atorvastatin 10 mg 1 tab QOD, Bisoprolol 5 mg 1 tab BID.
The patient reported that breast gigantism had been occurred within the past 3 years. He had never suffered from liver disease, diabetes mellitus, or alcoholism. Laboratory examination showed normal values of liver function, renal function, serum concentration of testosterone and estradiol: GOT was18 U/L (normal range (NR): 8-38 U/L), GPT was14 U/L (NR: 4-44 U/L), BUN was 9 mg/dL (NR: 8-20 mg/dL), testosterone was 4.57 ng/mL (NR: 2.7-10.7 ng/mL), estradiol was 30 pg/mL (NR: 8-36 pg/mL). Captopril was stopped after the visit and painful of nipple disappeared a week later.

Figure 1 Swelling & pain on bilateral breasts
In 2008 March, patient complained of duodenal discomfort and was given sulpiride 50 mg twice daily. Two months later, he complained of painful and swelling on bilateral breasts (as figure 1). His cardiologist asked for pharmacist intervention.
The patient's medication file was reviewed and it was concluded then on the possibility of sulpiride induced. Symptoms vanished after discontinuation of sulpiride. The Naranjo scale showed a probability event, the total score is 76,7.
Discussion and management objectives
Gynecomastia was defined as an abnormal accumulation of tissue in the male breast. It is a normal physiologic finding in 3 groups: newborns (60-90%), in whom it is transient due to the exposure to maternal estrogens; adolescents (4-69%), who experience a transient condition in association with puberty; elderly (24-65%), in whom it is due to decreased androgenic activity8,9.
The prevalence of dug induced gynecomastia is estimated 10-25%8. Patients complain of tenderness and painful or inflammation on bilateral breasts. Serum prolactin level is one of the important indicators which can be used to exclude the pathologic related causes. In pharmacologic related gynecomastia, the serum prolactin level is commonly within normal range. Prolactin does not stimulate breast tissue growth directly. Hyperprolactinemia has been associated with gynecomastia, probably plays an indirect role by causing hypogonadism, but the main cause is pituitary prolactin-secreting adenoma.
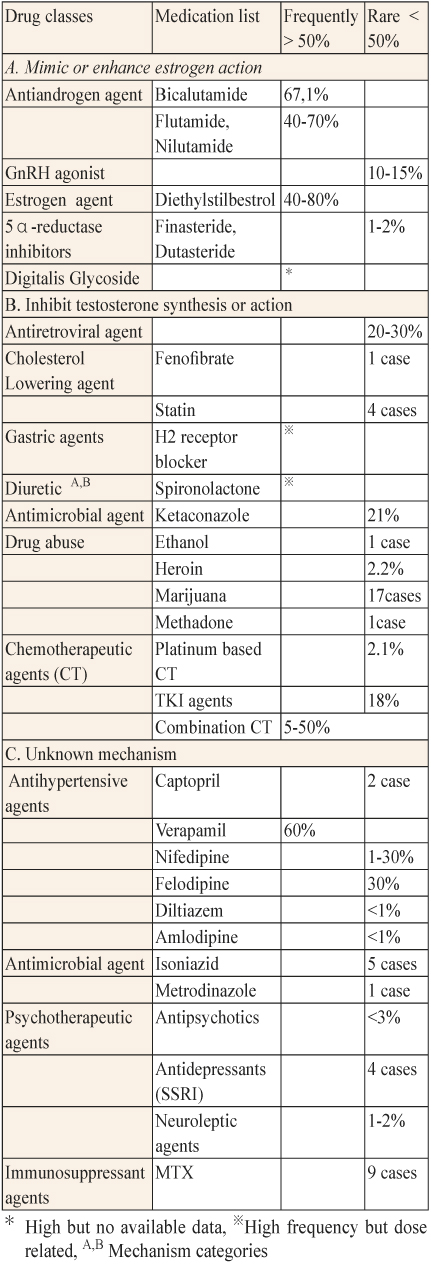
The pathophysiologic mechanism in drug related gynecomastia is categorized as 3 parts: A. Mimic or enhance estrogen action such as exogenous estrogens for the treatment of prostate cancer or antiandrogens. B. Inhibit testosterone synthesis or action. C. Act by unknown mechanism which includes the majority of agents, our case report is one of the medications include in this group.
Exposure to certain substances, for example, an estrogen-containing cream designed to treat baldness, foods prepared from estrogen-treated animal, occupational exposure during the manufacture of estrogen-containing medications, drugs of abuse (i.e., marijuana), dietary supplementary such as phytoestrogen, although there are not apparent but have been reported may result in gynecomastia. We briefly review common causative agents, the mechanism categories and incidence frequency on Table 5.
Table 5. Drugs causing gynecomastia8-10
A thorough history and physical examination should be revealed to cases of likely drug-induced gynecomastia. The disorder may often resolve spontaneously (± 1 month) after discontinuing the offending drug during the painful proliferative phase. Pharmacotherapy may be helpful when symptoms of breast enlargement, pain, tenderness persist or patient asks for due to psychological embarrassment. Symptoms of pain and tenderness usually disappeared after 6-12 months, as fibrotic stage appear and replaces the proliferation of glandular tissue, surgical treatment is usually required.
There are two medications have been recommended to reduce the symptoms of gynecomastia, one is the antiestrogen Tamoxifen (20 mg/day) and the other is the aromatase inhibitor anastrazole (1 mg/day), but both agents are not approved by FDA for treatment of gynecomastia3.
Surgical intervention include subcutaneous mastectomy with or without associatopn liposuction, a simple surgical to reduce breast size and remove painfully enlarged tissue. Radiation therapy with a single dose of 10-15 Gy before hormonal therapy may ameliorate the risk of gynecomastia. Surgical or radiation therapy is often performed especially in cases resulting prostate cancer treatment.
Conclusion
There is no prevalence estimation of drug induced galactorrhea, but most review concluded significant increase in prolactin serum concentration is frequently associated with symptoms, and galactorrhea is one of it. Typical antipsychotic agents are frequently responsible for drug related hyperprolactinemia11.
Gynecomastia in men is a normal pathologic finding in some episodes in men's life, such as puberty, obesity. It is not easily detected by patient alone, unless symptoms show painfulness, tenderness or inflammation around the nipple or on bilateral/unilateral breast tissue appeared. The serum prolactin in gynecomastia do not always have elevated levels, but when hyperprolactinemia presents, it commonly leads to hypogonadism , because hyperprolactinemia decreases hypothalamic secretion of GnRH, resulting hypogonadism. Galactorrhea is not often occurred in men; commonly it signifies a serious underlying disorder.
Both of laboratory data and physical examination are strongly recommended to physicians to exclude pathology causes. Laboratory data include serum prolactin, estrogen and testosterone hormone level, thyroid-stimulating hormone level, follicle stimulating hormone and luteinizing hormone.
Physical examination includes a pituitary magnetic resonance imaging scan to exclude the possibility of pituitary adenoma.
Stop using the causative agents is strongly recommended. Patient with galactorrhea and normal/abnormal serum prolactin level do not require any specific treatment, unless they are bothered by the galactorrhea. Low dose of bromocriptine (Parlodel), a dopamine agonist, is preferred for most patients with hyperprolactinemia7,8. It is extremely cheap and effectiveness in lowering prolactin level, eliminating galatorrhea, restoring gonadal function, and decreasing tumor size. For those intolerant to bromoriptine, cabergoline is an alternative agent; it is an ergoline derivative with longer half-life than bromocriptine. The dopamine agonist application should be cautiously used in patients with psychotic disorder due to possible exarcebation of symptoms. Alternative antipsychotic agents with less induced hyperprolactinemia are recommended in this population12.
In medication related gynecomastia, during the proliferative phase, manifested clinically such as breast pain and tenderness, drug such as testosterone, dihydrotestosterone, danazol, clomiphene, tamoxifen, have been uncontrolled and thus can be difficult to interpret because gynecomasia can resolve spontaneously8. Testosterone replacement therapy should not be used unless patient is hypogonadal. In eugonadal men, testosterone usage may increase the risk of gynecomastia through aromatization of testosterone to estradiol.
Although it is not approved by FDA , randomized clinical trials suggest low dose tamoxifen (20 mg/day) indicates more effective than aromatase inhibitors and radiation therapy for antiandrogen related gynecomastia and breast pain or superior to a single radiation dose of 12 Gy in preventing gynecomastia10.
Medication induced breast abnormality in men are most often case reports of breast abnormality than in women. A number of potential pathophysiology mechanisms have been discussed but methods to evaluate are not currently available.
Thompson et al., (1993) considered drug-induced gynecomastia is difficult to prove conclusively because of the prevalence of gynecomastia as a normal finding was not considered; secondly, lack of standardized physical diagnostic criteria; and thirdly missing confirmatory data (i.e., drug rechallenge or physiologic mechanism)9.
摘要
藥品誘發乳房異常症狀
秀傳紀念醫院藥劑科藥師 陳培瑛、劉育伶、賴淑惠
彰濱秀傳紀念醫院藥劑科藥師 羅振旭
男性女乳症和乳漏症是兩種獨特發生在乳房的不良反應。許多藥物會導致不良反應發生。我們分別敘述藥物在男性與女性引起乳房異常的案例。
案例一是一位34歲的婦女,因胃食道逆流就醫,醫師給予 mosapride、lansoprazole and sulpiride 50毫克治療3個月,病人因乳漏、月經週期不規律等症狀到乳房外科就診,經血清檢查結果顯示泌乳素 (prolactin) 上升至84.0 ng/mL (正常範圍:5.8-26.53)。病人從未有任何內分泌學異常病史,因此主治醫師高度懷疑乳漏症與其服用藥品有關,建議停用 mosapride 和 lansoprazole 兩種藥品,並於一個月後複查患者的泌乳素,此時數值已在正常範圍內 (12.02 ng/mL)。
案例二是位男性病人在服用 captopril 兩年後主訴雙側乳腺腫大、乳頭觸痛 (captopril 的用藥紀錄是12.5毫克,一天兩次,使用2年後單次劑量增加為25毫克。此劑量只使用1個月)。血清檢查報告顯示肝、睪丸激素和雌二醇數值都在正常範圍內。因此停用 captopril,症狀大約一週後消失。一年後,乳房症狀又出現,經檢視病人服用藥物紀錄發現,病人因胃腸不適曾使用 sulpiride 50毫克每日兩次所導致的,停藥後症狀也逐漸消退。
以上兩例乳房之不良反應顯示相關症狀部分是屬於可逆的,目前最佳治療選擇是停用相關藥品並改使用其他替代藥品,詳細審查個案用藥史亦有助於確認是否是藥物不良反應。
Reference:
1. Perkins DO. Antipsychotic-induced hyperprolactinemia: Pathology and clinical consequence. Adv Stu Med. 2004; 4(10F):S982-6.
2. Izquierdo Prieto OM, Moreno Alia E, Rosillo Gonzalez A: Galactorrhea induced by lansoprazole. Aten Primaria. 2004; 34(6):325-6.
3. Jabbar A, Khan R, Farrukh SN: Hyperprolactinaemia induced by proton pump inhibitor. J Pak Med Assoc. 2010; 60(8):689-90.
4. Torre DL, Falorni A: Pharmacological causes of hyperprolactinemia. Ther Clin Risk Manag 2007;3(5) 929-51.
5. Alexander Leung K.C, Pacaud D: Diagnosis and Management of Galactorrhea. Am Fam Physician 2004;70(3):543-50.
6. Markusse HM, Meyboom RH: Gynaecomastia associated with captopril. Br Med J 1988; 296(6631):1262-3.
7. Nakamura Y, Yoshimoto K, Saimasi: Gynaecomastia induced by angiotensin converting enzyme inhibitor. BMJ 1990; 300(6723):541.
8. Eckman A, Dobs A: Drug-induced Gynecomastia. Expert Opinion Drug Safety 2008;7(6):691-702.
9. Thompson DF, Carter JR: Drug-induced Gynecomastia. Pharmacotherapy 1993; 13(1):37-45.
10. Bowman JD, Kim H, Bustamante JJ: Drug-induced Gynecomastia. Pharmacotherapy 2012; 32(12):1123-1140.
11. Wieck A, Haddad PM: Antipsychotic-induced hyperprolactinemia in women: pathophysiology, severity and consequences: Selective literature review. The Br J Psychiatry 2003;182:192-204.
12. Carroll RW, Christodoulou P, Baynes KC; et al: Hyperprolactinemia in a Patient with a Pituitary Adenoma Receiving Antipsychotic Drug Therapy. J Psychiatr Pract 2012;18(2):126-9.