摘要
胃癌是世界第五大癌症,癌症死亡率排名第三,衛福部國健署於105年4月公布102年癌症發生統計報告,發生率的排名於男性為第7位、女性為第10位,新增個案3,768位。胃癌組織型態以腺癌為主,非腺癌相對少見。胃癌危險因子有幽門桿菌感染、抽菸、鹽分攝取過多和重度飲酒。診斷出胃癌時多半已經是無法手術或轉移性之胃癌,此時第一線化學治療可選用之藥品有 fluorouracil、capecitabine、cisplatin、oxaliplatin、carboplatin、docetaxel、irinotecan、epirubicin 和 UFUR;有 HER-2/Neu (human epidermal growth factor receptor 2) 陽性的病人應加上 trastuzumab,可延長存活,65歲以上晚期胃癌病人,選用 fluorouracil、leucovorin 和 oxaliplatin (FLO) 延長存活較 FLP (fluorouracil、leucovorin 和 cisplatin) 佳;XELOX 處方整體反應率高,毒性小,是胃癌常見的藥品組合。
關鍵字: 胃癌、化學治療、metastatic gastric cancer、advanced gastric cancer
壹、前言
胃癌是世界第五大癌症,癌症死亡率排名第三,衛福部國健署於105年4月公布102年癌症發生統計報告,胃惡性腫瘤發生個案數占全部惡性腫瘤發生個案數的3.80%,當年因此惡性腫瘤死亡人數占全部惡性腫瘤死亡人數的5.00%。發生率的排名於男性為第7位、女性為第10位;死亡率的排名於男性為第6位、女性為第5位,民國102年初次診斷為胃惡性腫瘤者共計3,768人1。
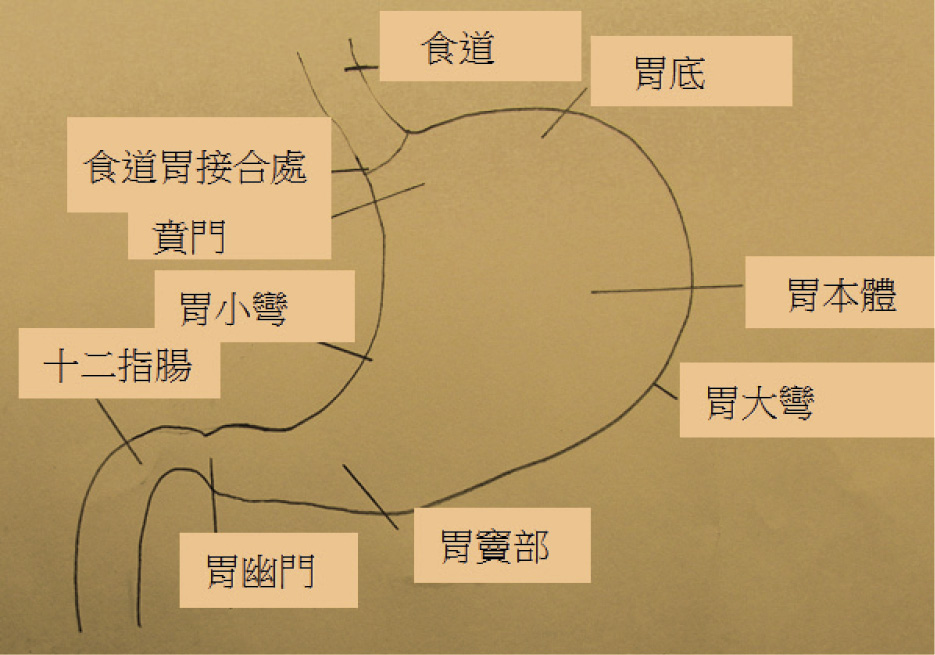
胃癌有發生於肌肉層的胃平滑肌癌、神經源型的胃神經細胞瘤、黏膜內的胃惡性淋巴瘤及源自黏膜層腺體細胞變異之胃腺細胞癌。一般所稱胃癌係指胃腺癌,佔胃部惡性腫瘤約90%,胃癌組織型態男、女性病人均以腺癌最多,分別占男性個案之90.63%,女性個案之87.96%2。胃癌一般分為腸道型 (intestinal type,癌細胞具腺體樣式,分化較好) 和彌漫型 (diffuse type,癌細胞不成腺體排列,成單一細胞或小堆瀰漫散佈),不同癌變型態將影響治療的選擇,例如腸道型 HER-2/Neu 陽性比率較瀰漫型高。胃癌危險因子有幽門桿菌感染、抽菸、鹽分攝取過多與重度飲酒,其中重度飲酒易引起「非賁門」區的胃癌 (圖一)。
圖一 胃解剖圖
根據我國102年癌症登記報告診斷出胃癌時的期別以第四期佔26.57%最多,NCCN 指引2017年第1版,提到局部晚期或轉移性胃癌病人,化療可以緩解症狀,比支持性療法有更好的存活率和生活品質3,因此,本文整理無法手術或轉移性胃癌化療相關研究,一探各種第一線化療組合對整體存活率的效果、毒性、反應率及適用族群。
貳、藥品組合
對於已經是無法手術或轉移性胃癌,此時化學治療可選用之藥品有 fluorouracil、capecitabine、cisplatin、oxaliplatin、carboplatin、docetaxel、irinotecan、epirubicin3和 UFUR,有 HER-2/Neu (human epidermal growth factor receptor 2) 陽性的病人可用 trastuzumab 延長存活。
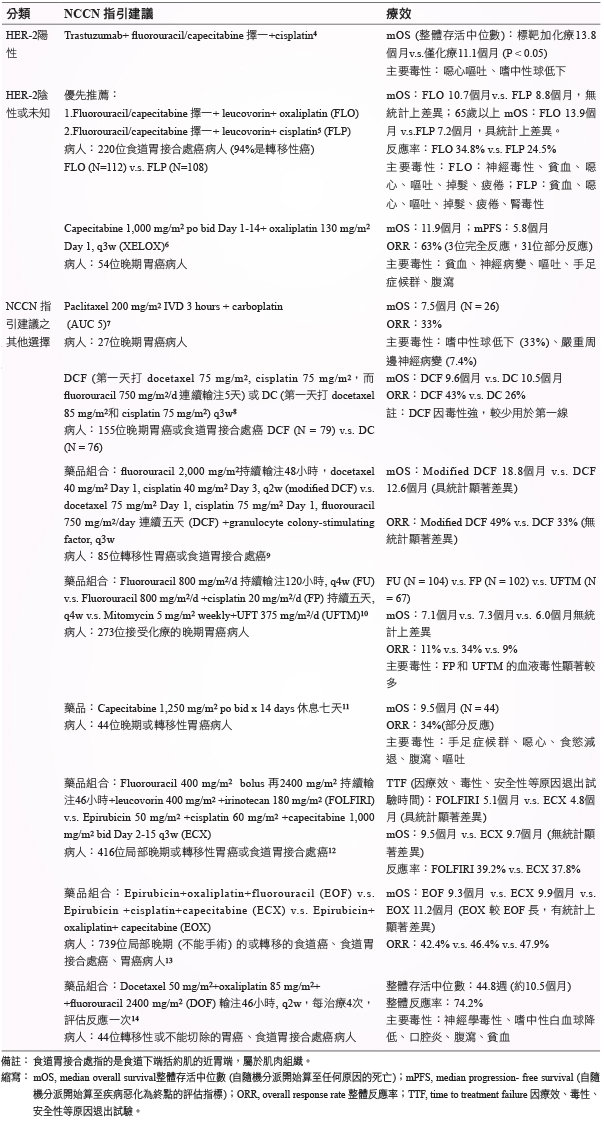
根據美國國家癌症資訊網 National Comprehensive Cancer Network (NCCN) 指引,無法切除的局部晚期、復發或轉移的胃癌治療組合 (表一)。
表一 無法切除的局部晚期、復發或轉移的胃癌第一線治療組合 (NCCN 指引建議)3
參、討論
根據研究,胃癌 HER-2陽性的比例介於9-27%之間,HER-2陽性的比例與人種較無關係,與腫瘤部位、組織學、腫瘤分化程度有關,例如 ToGA 試驗中3,HER-2陽性的比例,食道胃接合處癌33%,胃部腺癌21%,中度分化 (moderately differentiated) 又高於分化不良者 (poorly differentiated),HER-2陽性的比例在腸道型 (intestinal histology) 又比瀰漫型或混合型 (diffuse/mixed histology) 多,因此將胃腺癌依據組織病理再區分為腸道型 (癌細胞具腺體樣式,分化較好) 或瀰漫型 (癌細胞不成腺體排列,成單一細胞或小堆瀰漫散佈),將可望提供治療方向。HER-2陽性者,如晚期胃癌或食道胃接合點癌,對 trastuzumab 有反應的病人,以傳統化療併用 trastuzumab 可望延長整體存活中位數2.7個月。
HER-2陰性或未知的轉移性胃癌病人,NCCN 指引推薦 fluorouracil + leucovorin+ oxaliplatin (FLO) 或口服 capecitabine+ oxaliplatin (XELOX) 或 fluorouracil 或capecitabine+ leucovorin+ cisplatin (FLP) ,尤其是65歲以上的病人,採用 FLO 比起 FLP,前者存活中位數多6.7個月,同時 FLO 與 XELOX 在安全性的表現較 FLP 佳3。其他處方中,docetaxel 40 mg/m2 Day 1, cisplatin 40 mg/m2 Day 3, fluorouracil 2,000 mg/m2持續輸注48小時 (modified DCF) q2w,在存活中位數表現優異,然而安全性較 DCF (docetaxel 75 mg/m2 Day 1, cisplatin 75 mg/m2 Day 1, fluorouracil 750 mg/m2/day 連續五天) 差,支持文獻人數較少,因此並未放在優先推薦名單之中3。三種化療藥的組合,如 modified DCF、DCF、Epirubicin+oxaliplatin+fluorouracil (EOF)、Epirubicin +cisplatin+capecitabine (ECX)、Epirubicin+ oxaliplatin+ capecitabine (EOX) 等,主要用於日常體能狀況較佳的病人,兩種化療藥組合的處方因為毒性較低而較常使用。
NCCN 指引沒有收錄日本開發的藥物如 TS-1 (Tegafur/gimeracil/oteracil),健保給付規定為胃癌術後輔助性化療,用於罹患 TNM StageⅡ (排除 T1)、ⅢA 或 ⅢB 胃癌且接受過胃癌根除性手術的成年患者,限用1年,暫不在本篇討論之列。另一個日本藥 UFUR (Uracil-Tegafur) ,健保給付規定可用於轉移性胃癌。UFUR 與葉酸搭配使用,反應率約16-29%之間,整體存活中位數只有5.8個月,因此通常不單獨使用來治療轉移性胃癌,有學者建議可由 UFUR 搭配其他化療藥品 (epirubicin 或 cisplatin 等) 可用於取代 fluorouracil15,另外也可用於病況較差時的緩和性治療。
肆、結論
轉移性胃癌的病人,在治療前應進行 HER-2檢測,藉以決定是否加入 trastuzumab,大於65 歲以上的轉移性胃癌病人,採用每兩週住院施打一次的 FLO (fluorouracil, leucovorin 和 oxaliplatin) 比起 FLP (fluorouracil, leucovorin 和 cisplatin),前者存活中位數可望延長6.7個月 (意即搭配 oxaliplatin 比 cisplatin 好),安全性上表現較 FLP 佳;XELOX (capecitabine 1,000 mg/m2 po bid Day 1-14+ oxaliplatin 130 mg/m2 Day 1, q3w) 處方整體反應率達63%,且毒性低、整體存活期11.9個月6,是臨床上最常見的轉移性胃癌第一線口服化療組合,但因治療效果與病人服藥配合度有關,而臨床試驗的服藥配合度一般比現實生活高,藥師應提醒病人規則服藥才能有預期的療效。
Introduction of Systemic Therapy for Unresectable Locally Advanced, Recurrent or Metastatic Gastric Cancer
Hung-Yi Chen1, I-Ting Liu2
Department of Pharmacy, National Cheng Kung University Hospital1
Division of Hematology and Oncology, Department of Internal Medicine,
National Cheng Kung University Hospital2
Abstract
Gastric cancer is estimated the fifth most frequently diagnosed cancer and the third leading cause of death from cancer worldwide. In April 2016, health promotion administration, ministry of health and welfare announced cancer statistics of 2013. There were 3,768 new cases of gastric cancer in Taiwan and gastric cancer was ranked at the 7th for men and at the 10th for women among all types of cancers.
Adenocarcinoma is the most common type of gastric cancer while non-adenocarcinoma is relatively rare. Risk factors of gastric cancer include Helicobacter pylori (H. pylori) infection, smoking, high salt intake and heavy alcohol drinking. Gastric cancer is often diagnosed at an advanced stage (unresectable locally advanced or metastatic). Available chemotherapy agents include fluorouracil, capecitabine, cisplatin, oxaliplatin, carboplatin, docetaxel, irinotecan, epirubicin, and UFUR. In patients with HER-2/Neu (human epidermal growth factor receptor 2) positive gastric cancer, there was a significant improvement in the median overall survival with the addition of trastuzumab to chemotherapy compared to chemotherapy alone. In older adult patients (> 65 years old), fluorouracil, leucovorin and oxaliplatin combination (FLO) seemed to be associated with better overall survival than fluorouracil, leucovorin and cisplatin combination (FLP). XELOX regimen is often used to treat advanced gastric cancer because of high overall response rate and less toxicity.
參考資料:
1. https://gene.hpa.gov.tw/index.php?mo=DiseasePaper&action=paper1_show&cate=Set1&csn=64&sn=458.
2. http://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=269&pid=5191.
3. https://www.nccn.org/professionals/physician_gls/pdf/gastric.pdf
4. Bang YJ, Van Cutsem E, Feyereislova A, et al: Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet. 2010; 376 (9742): 687-97.
5. Al-Batran SE, Hartmann JT, Probst S, et al: Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. J Clin Oncol 2008;26:1435-1442.
6. Park YH, Lee JL, Ryoo BY, et al: Capecitabine in combination with oxaliplatin (XELOX) as a first-line therapy for advanced gastric cancer. Cancer Chemother Pharmacol. 2008; 61(4): 623-9.
7. Gadgeel SM, Shields AF, Heilbrun LK, et al: Phase II study of paclitaxel and carboplatin in patients with advanced gastric cancer. Am J Clin Oncol. 2003; 26(1): 37-41.
8. Ajani JA, Fodor MB, Tjulandin SA, et al: Phase II multi-institutional randomized trial of docetaxel plus cisplatin with or without fluorouracil in patients with untreated, advanced gastric, or gastroesophageal adenocarcinoma. J Clin Oncol. 2005; 23(24): 5660-7.
9. Shah MA, Janjigian YY, Stoller R,et al: Randomized multicenter phase II study of modified docetaxel, cisplatin, and fluorouracil (DCF) versus DCF plus growth factor support in patients with metastatic gastric adenocarcinoma: a study of the US gastric cancer consortium. J Clin Oncol. 2015; 33(33): 3874-9.
10. Ohtsu A1, Shimada Y, Shirao K, et al: Randomized phase III trial of fluorouracil alone versus fluorouracil plus cisplatin versus uracil and tegafur plus mitomycin in patients with unresectable, advanced gastric cancer: The Japan Clinical Oncology Group Study (JCOG9205). J Clin Oncol. 2003; 21(1):54-9.
11. Hong YS, Song SY, Lee SI, et al: A phase II trial of capecitabine in previously untreated patients with advanced and/or metastatic gastric cancer. Ann Oncol 2004; 15: 1344-1347.
12. Guimbaud R, Louvet C, Ries P, et al: Prospective, randomized, multicenter, phase III study of fluorouracil, leucovorin, and irinotecan versus epirubicin, cisplatin, and capecitabine in advanced gastric adenocarcinoma: a French intergroup (Fédération Francophone de Cancérologie Digestive, Fédération Nationale des Centres de Lutte Contre le Cancer, and Groupe Coopérateur Multidisciplinaire en Oncologie) study. J Clin Oncol. 2014; 32(31): 3520-6.
13. Cunningham D, Starling N, Rao S, et al: Capecitabine and oxaliplatin for advanced esophagogastric cancer. N Engl J Med 2008; 358: 36-46.
14. Shankaran V, Mulcahy MF, Hochster HS, et al: Docetaxel, oxaliplatin, and 5-fluorouracil for the treatment of metastatic or unresectable gastric or gastroesophageal junction (GEJ) adenocarcinomas: Preliminary results of a phase II study. Gastrointestinal Cancers Symposium 2009: Abstract 47.
15. Aykan NF, Idelevich E. The role of UFT in advanced gastric cancer. Ann Oncol. 2008; 19(6): 1045-52.
通訊作者:陳弘益/通訊地址:台南市北區勝利路138號
服務單位:成大醫院藥劑部藥師/聯絡電話:(O) 06-2353535 ext 6505