心臟衰竭之血壓處理與治療
張羽汶、邱春吉、戴慶玲
高雄長庚紀念醫院藥劑部
摘要
高血壓是心臟衰竭病人常見的共病症,多數可改善心衰竭病人預後之藥物具有潛在的降壓作用。然而,降血壓和心衰竭臨床治療結果的關聯性尚未明確。面對低射出分率心衰竭( heart failure with reduced ejection fraction, HFrEF )病人,臨床指引推薦以符合心衰竭適應症的藥物治療高血壓,血壓目標值為130/80mmHg。面對正常射出分率心衰竭( heart failure with preserved ejection fraction, HFpEF )病人,臨床指引尚未建立標準治療對策,因此傾向比照低射出分率心衰竭治療。低血壓的心衰竭病人,若可耐受藥物並無副作用發生,盡可能由低劑量調升至具改善心衰竭預後之藥物治療劑量。對於老年人,糖尿病、慢性腎臟病和心房纖維顫動等病人,血壓控制應有個別化的考量。由於心衰竭病人常合併多種共病症,增加治療複雜度,因此在處理血壓控制問題,需更多實證資料來佐證。
關鍵字: 心臟衰竭、高血壓、共病症、HFrEF
壹、前言
高血壓是心臟衰竭病人常見的共病症,可改善心衰竭病人預後的藥物如ACEI (angiotensin converting enzyme inhibitor)、ARB (angiotensin receptor blocker)、Beta-blocker、MRA (mineralocorticoid receptor antagonist) 等具有降壓作用。然而,降血壓和心衰竭臨床治療結果的關聯性尚未明確。本文以目前臨床實證為指引,探討心臟衰竭病人之血壓處理與治療。
貳、高血壓與心臟衰竭
高血壓定義為血壓大於140/90mmHg,是引發心臟衰竭的主要危險因素之一1。相較於低射出分率心衰竭(heart failure with reduced ejection fraction, HFrEF),血壓升高更常見於正常射出分率心衰竭(heart failure with preserved ejection fraction, HFpEF),盛行率高達90%2。在一般族群,血壓升高和心血管事件之間呈現線性相關;然而,有觀察性研究指出,收縮壓與心竭病人總死亡率和心血管死亡率之間呈現J型相關性,特別是HFrEF病人3。關於J型矛盾相關性,有學者認為非常低的收縮壓本身可能是有害的,當收縮壓低於110mmHg,即使已給予心衰竭藥物治療,仍會增加心衰竭住院風險4。反之,有學者認為低血壓是嚴重心臟功能異常和低心臟輸出之一替代指標,心臟本身異常才是造成臨床結果惡化主因,而非低血壓5。HFpEF者血壓與臨床結果之間的關聯性更不明確,低收縮壓或舒張壓是否導致不良預後,在觀察性研究中顯現不一致的報告6。因此,臨床醫師須於處方具心衰竭預後效益之藥物與潛在引發低血壓副作用的風險間尋求平衡3。
參、臨床指引推薦於心臟衰竭之高血壓治療
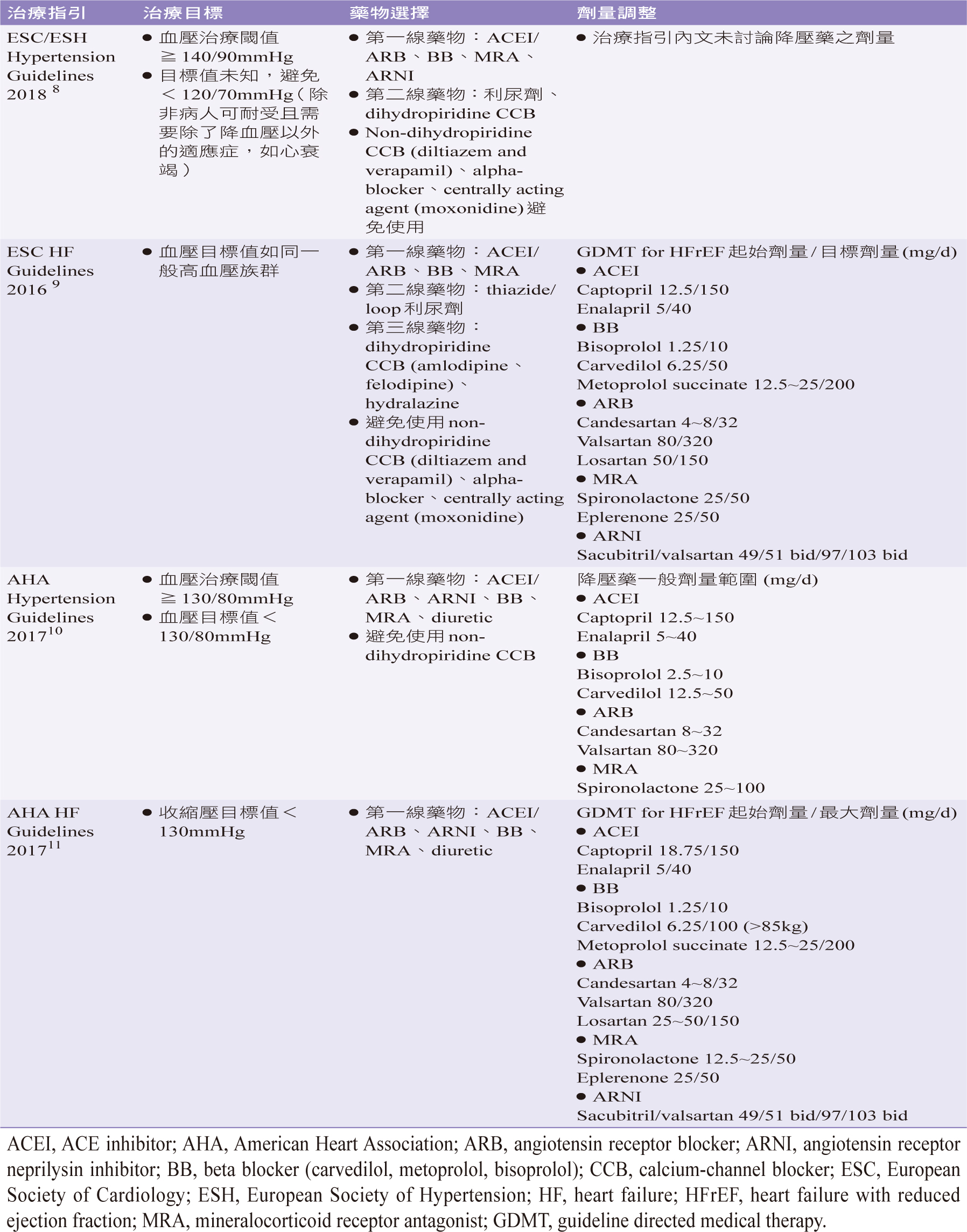
穩定控制血壓是心衰竭治療要素之一。迄今仍沒有臨床試驗研究心衰竭族群使用不同降血壓藥物的療效與治療目標。因此,治療建議是外推自其他高危險族群,顯示加強降壓可能增加副作用風險,但可呈現更大的心血管保護作用7。由於左心室射出率 ( left ventricular ejection fraction, LVEF )嚴重度顯著影響抗高血壓治療。因此,心衰竭指引建議在血壓處理區分為HFrEF和HFpEF,綜合各臨床指引有關心衰竭病人高血壓之處理建議摘要(表一)3,8-11、(表二)3,8-11。
肆、低射出分率心衰竭
ACEI、ARB、beta-blocker、MRA、ARNI (angiotensin receptor neprilysin inhibitor)等藥物皆具降壓作用,也被證實可減少HFrEF病人心血管疾病發生率與總死亡率,但這些好處是否是因降壓作用所引起的仍有爭議,可能是來自於神經體液調控(neurohumoral modulation)效益。雖然治療指引建議HFrEF使用的藥物對於降壓的臨床影響尚不明確,但心衰竭和高血壓指引針對降壓的臨床重要性仍具一致性看法,尤其是將改善HFrEF預後的藥物作為第一線治療選擇(表一)3,8-11。將兩種RAAS (renin angiotensin aldosterone system) 抑制劑如ACEI和ARB併用是禁忌,可能增加腎臟不良事件的風險。Non-dihydropyridine鈣離子通道阻斷劑(calcium channel blocker, CCB)和alpha-blocker會減弱心臟收縮力,應避免使用。Hydralazine和dihydropyridine CCB無法改善預後,但對於HFrEF是安全的,可作為降壓的附加用藥。藥物取代建議是以可耐受且無副作用發生為前提,漸進上調劑量,至可改善臨床結果 (表一)3,8-11。控制指標依2018 ESC/ESH(European Society of Cardiology/European Society of Hypertension)高血壓指引建議,保守的血壓目標值為低於130/80 mmHg,但不要低於120/70 mmHg8。其它指引並未特別標示血壓目標值。
表一 HFrEF病人高血壓之處理建議摘要3, 8-11
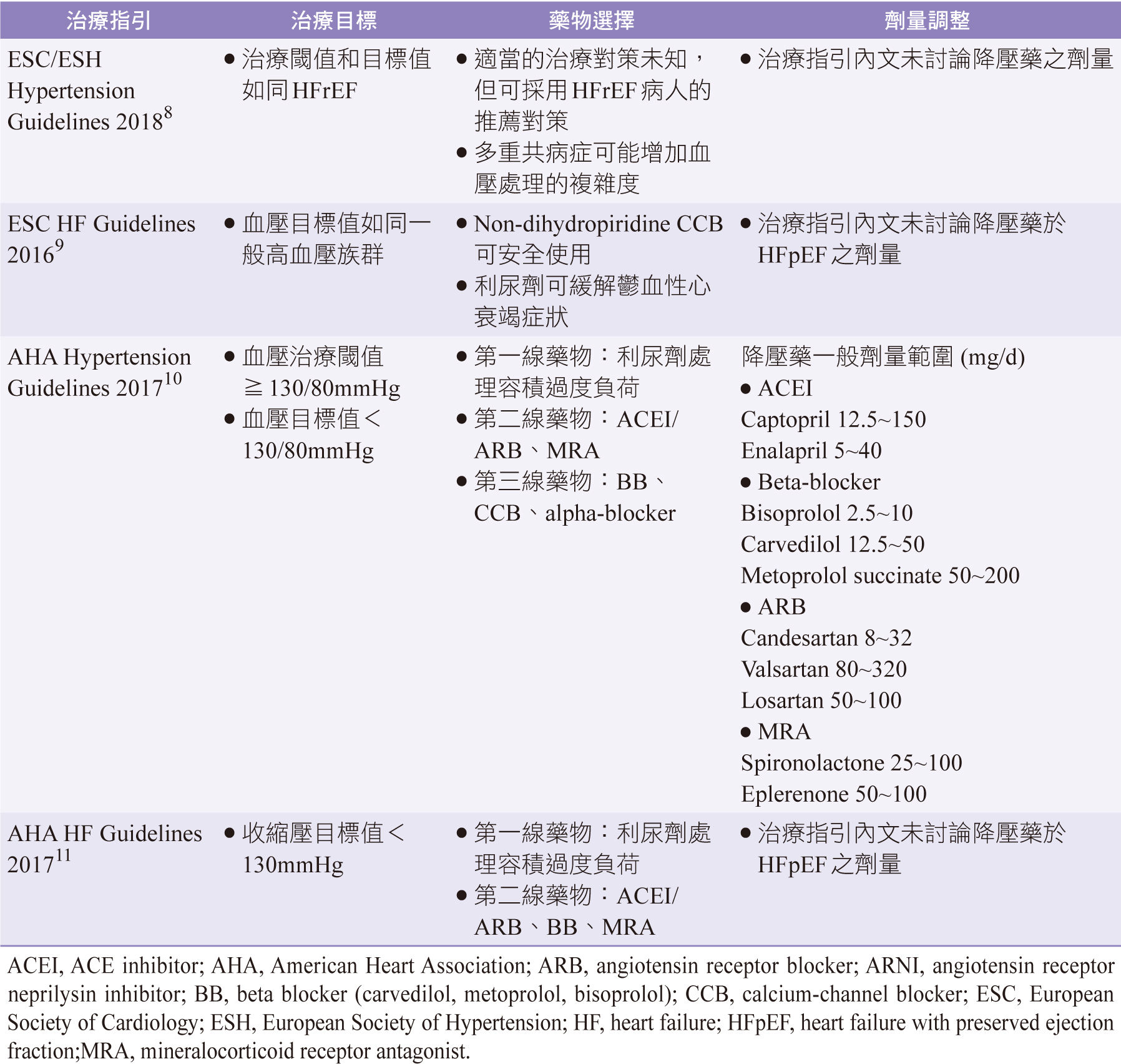
伍、正常射出分率心衰竭
迄今未有藥物顯示可減少HFpEF病人之發病率或死亡率,主要治療目標為緩解症狀和改善生活品質。雖然極少有關HFpEF病人的高血壓治療研究,但指引建議ACEI/ARB、MRA可作為第一線治療選擇(表二)3,8-11。利尿劑可處理體液滯留問題,是心衰竭治療重要處方藥物,不當過量使用可能造成血容量耗損,增加低血壓、腎功能受損、電解質異常等風險。其它降壓藥包括beta-blocker、CCB、alpha-blocker,建議作為第二、三線用藥。因此降壓藥選擇應考量病人共病症、耐受性與遵醫囑性等因素來執行。
表二 HFpEF病人高血壓之處理建議摘要3, 8-11
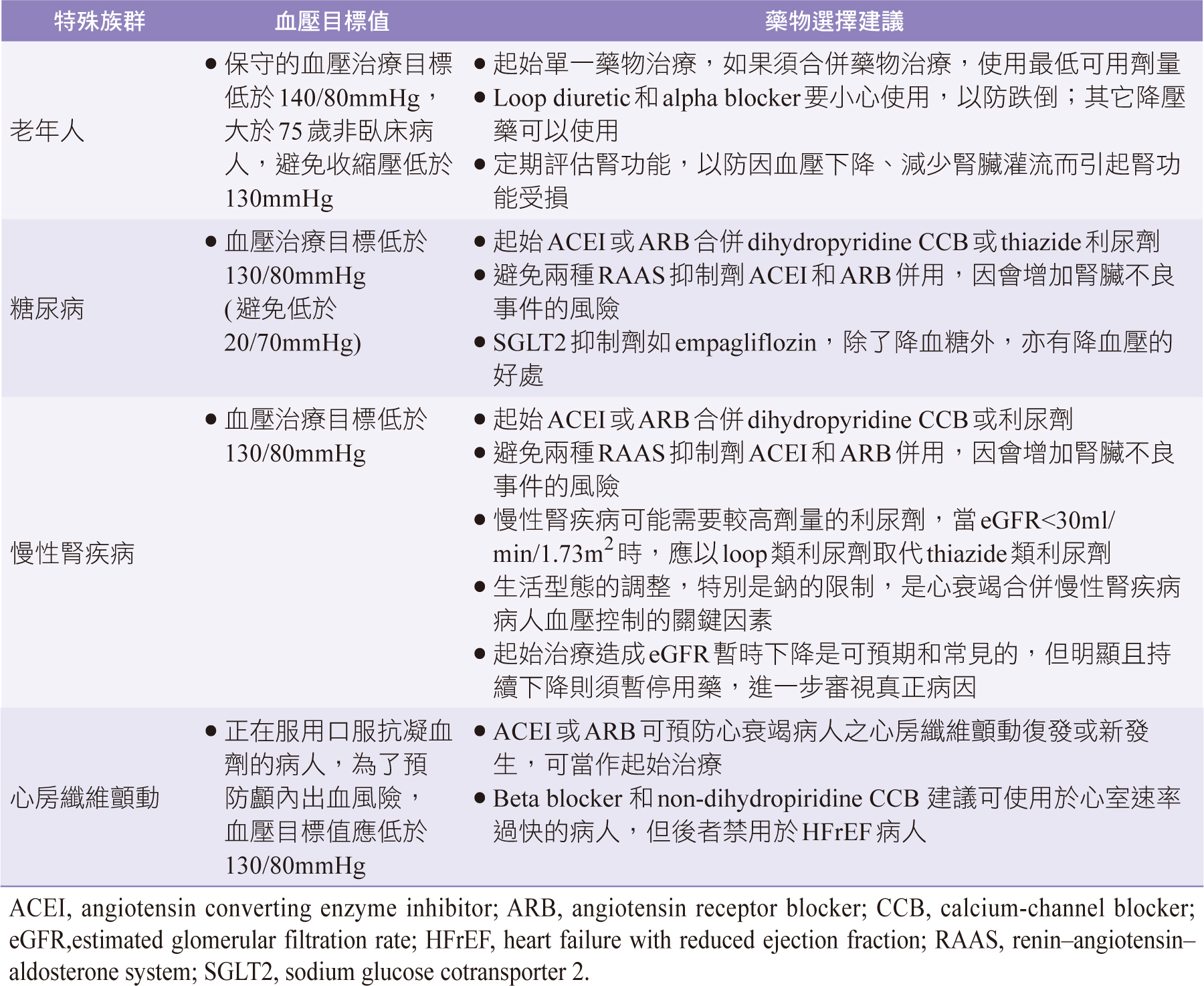
陸、特殊族群 (相關建議摘要如表三3,8-10)
一、老年人
尚無研究指出不同類降壓藥物在心血管事件的保護作用會因年齡而有差異。老年人由於保持血壓恆定和維持生命器官灌流能力受限,同時存在共病症,應個別化調整用藥。治療指引建議即使無法達到血壓控制目標,降低血壓仍與主要心血管事件和死亡率減少相關。
二、糖尿病
有無合併糖尿病之HFrEF病人,其治療在減少死亡率與罹病率之效果相同12。不同類降血糖藥物對於影響代謝和控制血糖的能力有差異,如SGLT2 (sodium glucose cotransporter 2)抑制劑,亦有降血壓的好處13。此外,DAPA-HF (dapagliflozin and prevention of adverse outcomes in heart failure)顯示無論有無糖尿病,HFrEF病人服用dapagliflozin相較於對照組,可降低心衰竭惡化或心血管死亡的風險14。心衰竭病人無論有無糖尿病,起始治療藥物應包含ACEI或ARB,因為此類藥物能更有效地減少白蛋白尿和延緩糖尿病腎病變惡化。相關建議摘要整理如表三3,8-10。
表三 心衰竭特殊族群病人高血壓之處理建議摘要3, 8-10
三、慢性腎臟病
若初始降壓藥物為RAAS抑制劑,由於血壓的下降會減少腎臟灌流壓,預期且常見暫時減少腎絲球濾過率,但在幾週後腎絲球濾過率下降情形會趨於穩定,不會造成實際腎損傷,因此密切觀察即可,無須停止治療。然而當腎功能超乎預期地顯著持續下降,則須停藥,進一步審視真正病因。
四、心房纖維顫動
心房纖維顫動 (atrial fibrillation, AF) 是心衰竭最常見的心律不整,而高血壓是前二者最常見的共病症,會明顯增加心血管事件的風險。治療高血壓可減少25%心衰竭病人新生AF風險15。雖然受限於實證數據,治療指引仍建議RAAS抑制劑可做為預防AF發生之降壓藥。Beta blocker或non-dihydropyridine CCB(diltiazem、verapamil)建議可用於心搏過速者,但non-dihydropyridine CCB因具有減弱心臟收縮力 (negative inotropic effect)和惡化心衰竭的風險,應避免使用於HFrEF病人9。
柒、結論
目前ESC、AHA (American Heart Association)之高血壓與心衰竭等治療指引皆一致建議使用符合心衰竭適應症且具降壓作用之藥物治療高血壓。由於缺乏實證數據佐證,理想的血壓目標值仍待確立。一般建議血壓目標值為130/80mmHg。在心衰竭臨床治療上,藥物若可耐受且無副作用發生,盡可能由低起始劑量調升至具改善心衰竭預後效果之治療劑量。面對特殊族群,包括老年人、糖尿病、慢性腎疾病和心房纖維顫動等病人,血壓的控制應作個別化考量。目前治療指引建議外推於已患高血壓之高風險族群,與心衰竭族群不盡相同,且此類病人常合併多種共病症,增加治療複雜度,因此有關心衰竭病人之高血壓處理對策需要更多實證資料來佐證。
Management and Treatment of Blood Pressure in Heart Failure
Yu-Wen Chang , Chun-Chi Chiou , Ching-Ling Tai
Department of Pharmacy, Kaohsiung Chang Gung
Memorial Hospital
Abstract
Hypertension is a common comorbidity in patients with heart failure and most drugs that have demonstrated to improve prognosis in this population have the potential to reduce blood pressure. Nonetheless, the relationship between blood pressure and clinical outcomes and the relevance of blood pressure reduction in heart failure remains unclear. In patients with heart failure with reduced ejection fraction, guidelines consensually recommend treating hypertension with drugs that have compelling indications in heart failure, with a target blood pressure of 130/80 mmHg. Inpatients with heart failure with preserved ejection fraction, guidelines acknowledge that the optimal treatment strategy remains unclear and thus recommend adopting a similar treatment strategy to patients with reduced ejection fraction. In any case, low blood pressure should not deter uptitration of drugs otherwise indicated to improve prognosis in heart failure, provided that patients tolerate drugs without adverse events. Special considerations and treatment adjustments are needed in the elderly as well as in patients with diabetes, chronic kidney disease and atrial fibrillation. More evidence is needed on blood pressure management in patients with heart failure in general, in whom the increasing burden of multimorbidity adds further complexity to treatment.
參考資料:
1. AGBD 2016 Risk Factors Collaborators. Global, regional, and national comparative riskassessment of 84 behavioural, environmental and occupational, and metabolic risksor clusters of risks, 1990-2016: a systematic analysis for the Global Burden of DiseaseStudy 2016. Lancet 2017;390:1345-422.
2. Nichols GA, Reynolds K, Kimes TM, et al. Comparison of risk of re-hospitalization,all-cause mortality, and medical care resource utilization in patients withheart failure and preserved versus reduced ejection fraction. Am J Cardiol2015;116:1088-92.
3. Pinho-Gomes AC, Rahimi K.Management of blood pressure in heart failure.Heart 2019;105 (8):589-95.
4. Desai RV, Banach M, Ahmed MI, et al. Impact of baseline systolic blood pressure onlong-term outcomes in patients with advanced chronic systolic heart failure (insightsfrom the BEST trial). Am J Cardiol2010;106:221-7.
5. Messerli FH, Rimoldi SF, Bangalore S. The transition from hypertension to heart failure:contemporary update. JACC Heart Fail 2017;5:543-51.
6. Tsujimoto T, Kajio H. Low diastolic blood pressure and adverse outcomes in heart failure with preserved ejection fraction. Int J Cardiol2018;263:69-74.
7. Bohm M, Schumacher H, Teo KK, et al. Achieved blood pressure and cardiovascular outcomes in high-risk patients: results from ONTARGET and TRANSCEND trials. Lancet 2017;389: 2226-37.
8. Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. European heart journal 2018;39:3021-104.
9. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European journal of heart failure 2016;18:891-975.
10. Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: AReport of the American College of Cardiology/American Heart Association Task Force onClinical Practice Guidelines. Hypertension 2018;71:e13-e115.
11. Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Journal of the American College of Cardiology 2017;70:776-803.
12. Gilbert RE, Krum H. Heart failure in diabetes: effects of anti-hyperglycaemic drug therapy. Lancet (London, England) 2015;385:2107-17.
13. Wanner C, Lachin JM, Inzucchi SE, et al. Empagliflozin and Clinical Outcomes in Patients With Type 2 Diabetes Mellitus, Established Cardiovascular Disease, and Chronic Kidney Disease. Circulation 2018;137:119-29.
14. McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction.N Engl J Med 2019;381(21):1995-2008.
15. Emdin CA, Callender T, Cao J, et al. Effect of antihypertensive agents on risk of atrial fibrillation: a meta-analysis of large-scale randomized trials. Europace : European pacing, arrhythmias, and cardiac electrophysiology : journal of the working groups on cardiac pacing, arrhythmias, and cardiac cellular electrophysiology of the European Society of Cardiology 2015;17:701-10.
通訊作者:邱春吉/通訊地址:高雄市鳥松區大埤路123號
服務單位:高雄長庚紀念醫院藥劑部/聯絡電話:(O) 07-7317123 ext 6274