Asia Pacific Antimicrobial Stewardship Preceptorship Program
Genevie Wang1, Chun-Wen
Cheng2, Ting-Shu Wu2,
Cheng-Hsun Chiu3, Hsuan-Ling Hsiao1,4
1Department of Pharmacy, Linkou Chang
Gung Memorial Hospital
2Division of Infectious Diseases,
Department of Internal Medicine, Chang Gung
Memorial Hospital, Chang Gung University
3Molecular Infectious Disease
Research Center, Chang Gung Memorial Hospital,
Chang Gung University
4Department of Respiratory Therapy,
Chang Gung University
Abstract
A one-year Asia Pacific antimicrobial stewardship (AMS) preceptorship program was developed and implemented by Linkou Chang Gung Memorial Hospital (CGMH) in 2018 and healthcare professionals from several hospitals in the Philippines and Vietnam participated. The project aimed to equip the participants with not only expertise and leadership necessary for establishing and/or improving antimicrobial use, but also techniques on enhancing strategy implementation. It involved pre-training teleconferences, one-week multi-disciplinary AMS workshop at CGMH, post-training teleconferences and finally, the mentors traveled abroad to conduct on-site inspections. The purpose of this article is to share CGMH’s approach (i.e., from advance preparations to implementation and follow-up) on making the preceptorship program a success. The importance of engaging the pharmacist in such activities is also discussed herein.
Key words:antimicrobial resistance (AMR), antimicrobial stewardship program (ASP), antimicrobial stewardship preceptorship program
I. Introduction
Antimicrobial agents are one of the greatest medical advances of the 20th century, however, they are quickly becoming useless due to antimicrobial resistance (AMR) and the pipeline of antimicrobials under development is limited. We therefore are heading for a post-antibiotic era in which infections caused by AMR microorganisms are becoming insusceptible to antimicrobial agents1. With the misuse of antimicrobials in multiple sectors (healthcare, veterinary, agriculture), drug resistance is now a pervasive phenomenon worldwide. Infections caused by AMR microorganisms usually result in longer durations of hospital stay, higher mortality, and reduced labor efficiency, adversely impacting patients' health and well-being2. The extensive health and economic implications associated with antimicrobial resistance has made it one of the most pressing public health issues the world faces today3. Linkou Chang Gung Memorial Hospital (CGMH) spares no effort in combatting AMR. It has been the first in 2004 to develop and deploy a hospital-wide computerized antimicrobial approval system prospectively auditing the use of antimicrobial agents4. In 2006, a steering committee comprising experts in antimicrobial stewardship (AMS) was established and has now accumulated more than ten years of experience in improving antimicrobial use among the in-patient, out-patient, and emergency departments. Furthermore, Linkou CGMH was selected to serve as one of the regional demonstration centers assisting in the implementation of the nationwide Antimicrobial Stewardship Program (ASP) led by Taiwan's Centers for Disease Control (CDC) from 2013 to 2015. Over the past years, Linkou CGMH have applied the ‘One Health' concept in the implementation of AMS initiatives. AMS is important to address the problem of AMR, but efforts of workers across sectors at the local level are never sufficient alone5. The Lancet Infectious Diseases Commission and World Health Organization have highlighted the need for a collaborative approach to support resource-limited countries in optimizing antimicrobial use through education and stewardship6. As part of our determination to deliver on the commitment of addressing public health problems, we sought to advance the ASP at some hospitals in Southeast Asia using a multifaceted, interprofessional mentoring program designed to help pharmacists, physicians, and nurses in resource-limited settings implement ASP or improve existing ASP in their institutions.
II. Description of the Mentoring Program
The Asia Pacific AMS Preceptorship Program was an important segment of a bigger project which has the following objectives:
1. To sort out all the AMS initiatives Linkou CGMH has taken throughout the years and to disseminate the information through scholarly work.
2. To support CGMH's ID physicians, nurses, pharmacists, and medical technologists in completing additional training to specialize in AMS mentoring.
3. To develop a comprehensive AMS curriculum consisting of lectures and workshop sessions that is suitable for implementation in the AMS preceptorship program for hospitals overseas.
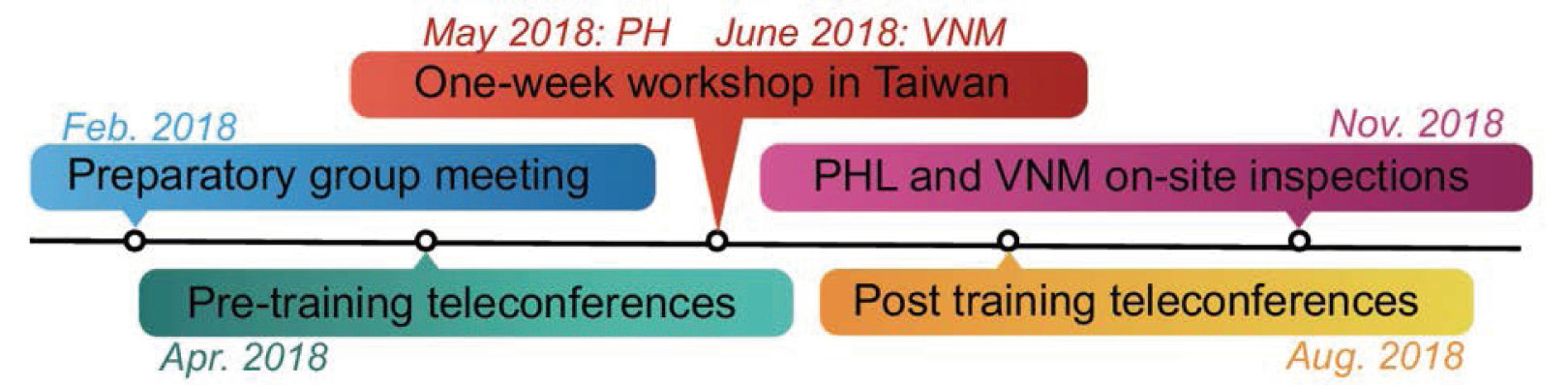
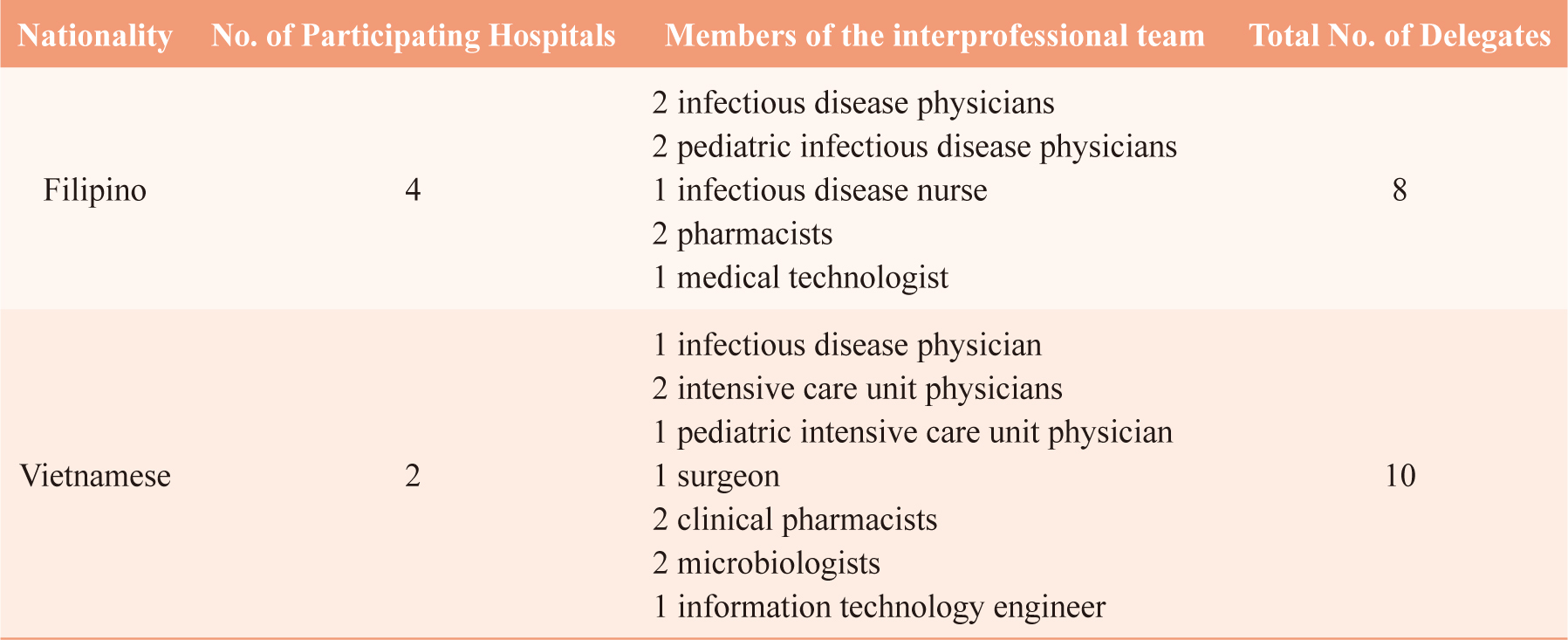
Training of two batches of foreign delegates began in 2018 (Figure 1). A total of 18 delegates from the Philippines (PHL) and Vietnam (VNM) were invited to participate in the mentoring program at no cost to the institution. The overall attendance was tabulated for presentation (Table 1).
Figure 1. Timeline of Events of the Asia Pacific AMS Preceptorship Program
Table 1. Attendance Breakdown of the Asia Pacific AMS Preceptorship Program
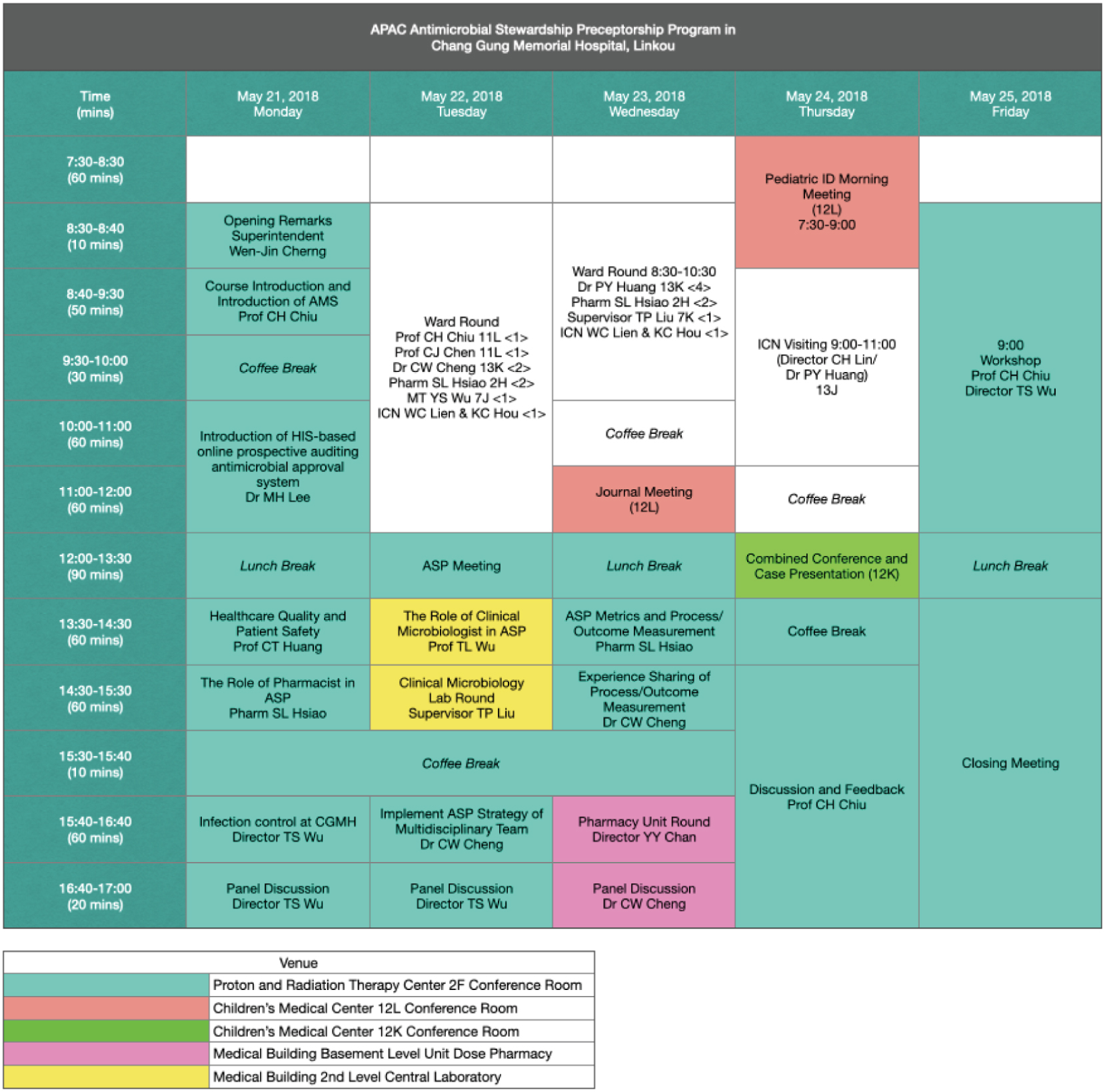
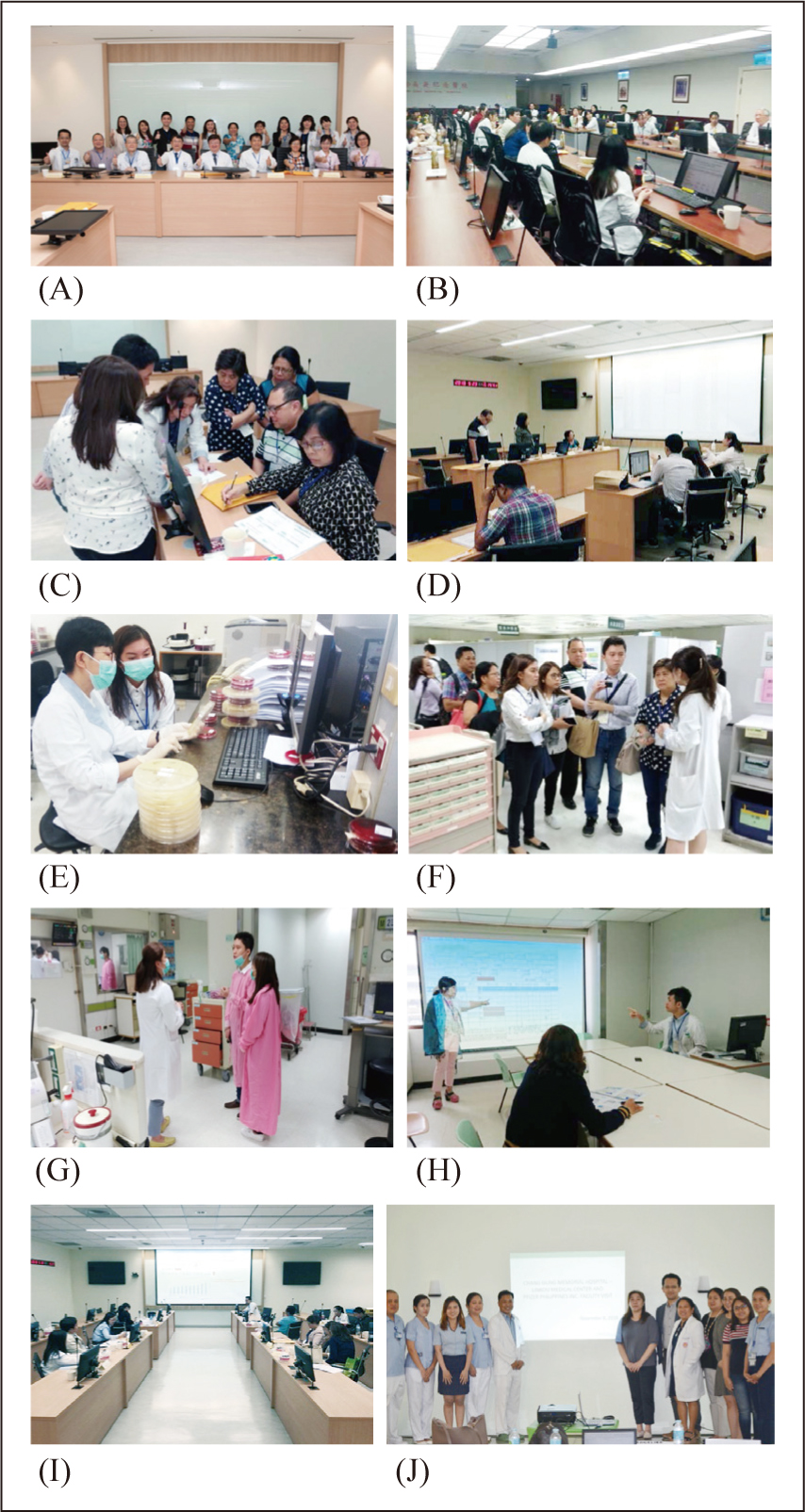
The AMS steering committee of Linkou CGMH served as the mentors and had several meetings to discuss the operations and logistics of the mentoring program before the official launch. In April, mentees were briefed via teleconference and were requested to provide mentors with information that describe current stewardship activities in their institutions. The mentees were finally welcomed to Linkou CGMH in May and June for their weeklong training on AMS, which consisted of lectures delivered in English, case discussions, hands-on activities, multidisciplinary ward rounds, pharmacy visit, and clinical laboratory tour. The Filipino and Vietnamese participants were trained on a separate schedule but with identical scope and content (Figure 2).
Figure 2. Weeklong Training Schedule
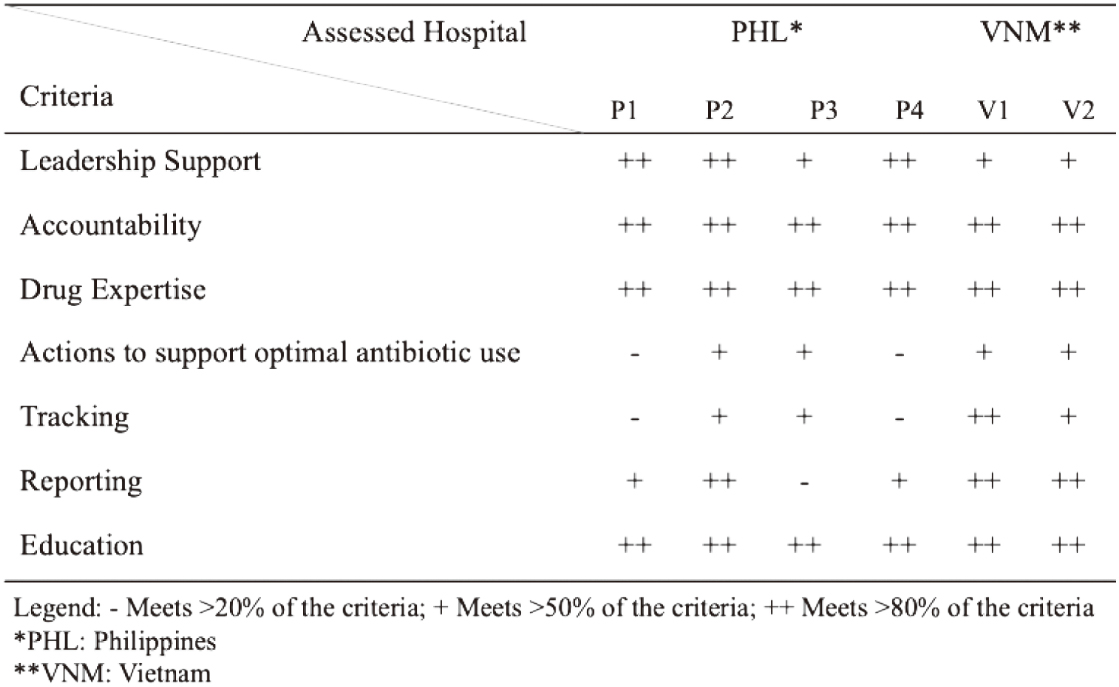
Soon after the weeklong training concluded, the mentors had regular follow-up teleconferences with the mentees to continually provide oversight on process improvement changes. At the end of the program, the mentors traveled abroad to conduct on-site inspections and the 2014 CDC checklist for core elements of hospital ASP was used to assess if necessary principles and actions to improve antimicrobial use were in place7.
III. Experience with the Program
In recent years, health authorities in Vietnam and the Philippines have been earnestly trying to further improve their regulatory landscape for antimicrobial stewardship. They have urged institutions to apply national guidelines and best practices for implementing and evaluating ASP. The mentors have observed that stewardship concepts were relatively easy for delegates to understand because they had some background on AMS before being accepted into the program. However, their information technology infrastructure and experience in outcomes measurement was inadequate.
The mentors placed emphasis on teaching ASP metrics and process/outcome measurement all throughout the weeklong training. During the last day, the participants got hands-on experience with generating and analyzing quantitative data on antimicrobial use to perform clinical and economic outcome analyses. The mentors also offered a strategy to overcome the lack of ASP-specific information technology; delegates were taught techniques on the surveillance of antimicrobial consumption using Microsoft Excel.
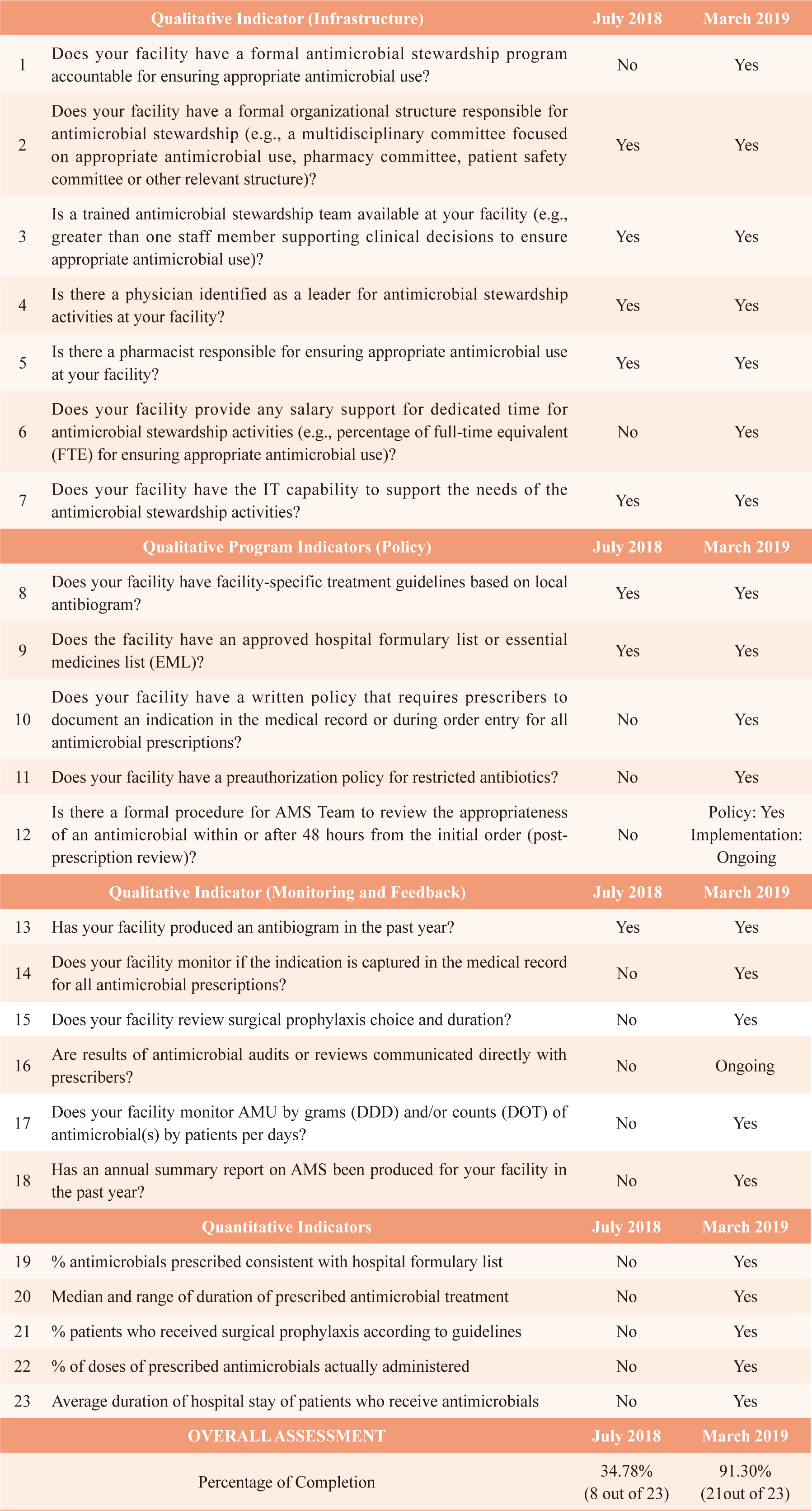
To ensure that the antimicrobial-related healthcare services of the hospitals involved in this program were meeting standards, the mentors were grouped into two pairs and each pair was sent abroad to conduct foreign site inspections in November 2018. Inspections were carried out around the 2014 CDC checklist for core elements of hospital ASP (Table 2). Non-conformities were dealt with straightaway and followed up accordingly to guarantee that areas for improvement were being addressed.
Table 2. An outline of the abridged 2014 CDC checklist for core elements of hospital ASP and the summarized results of the facilitators’ assessment
Even after the official ending of the project, contact with one particular hospital in the Philippines was not lost; they remain engaged with the mentors to discuss about their progresses and challenges in AMS implementation. Baseline and follow-up data documenting significant improvements was shared with the mentors (Table 3).
Table 3. Self-assessment of changes and progress in a hospital in the Philippines
IV. Insights and Lessons Learned
With pharmacists' expertise on and influence over antimicrobial use within the health system, they have a responsibility to take prominent roles in ASPs and participate in the infection prevention and control programs. However, the most important component of a pharmacist-driven ASP is the knowledge of the pharmacist in the area of infectious diseases (ID)8. Without beyond-basic understanding of ID and appropriate antibiotics for the treatment of specific infections, ASP pharmacists can face significant challenges in bringing a positive influence over antimicrobial use within the health system.
From the drafting of the project proposal to the planning, organizing, and implementation of this project, the pharmacists of Linkou CGMH have made enormous contributions. The pharmacist, member of the hospital's AMS team since its founding in 2006, hold a pivotal position in making this project a success. Not only did the pharmacist deliver lectures on the topics “The Role of the Pharmacist in ASP” and “ASP Metrics and Process/Outcome Measurement,” but also helped spearhead the project's all other pharmacy-related activities (i.e., pharmacy visit, hands-on workshop on antimicrobial consumption surveillance, conference calls, and the terminal foreign site inspections).
Currently, there are no standard, universally accepted metrics which reflect intervention effectiveness. Since the choice of metrics is primarily influenced by resource and data availability, an institution should tailor its choice of strategies to its needs and available resources. Sustained funding from the administration and enthusiastic medical staff support are also needed for program success9,10. While inaccessible electronic health records and other ASP-specific information technology make ASP implementation and surveillance difficult, unfamiliarity in the use of process/outcome measurement poses an even greater challenge. Mentoring by individuals with stewardship experience advances the learning curve, removes barriers limiting progress, and expedites the maturation of a stewardship program11.
Despite suffering setbacks that would have discouraged the implementation of effective ASP, the hospitals involved in this mentoring program still demonstrated commitment to support clinicians in daily stewardship duties and ensure successful antimicrobial-related outcomes. Their willingness to learn from each other's stewardship successes and failures continues to foster collaboration. Linkou CGMH is obligated to continually provide support and practical recommendations for hospital staff both locally and abroad, especially in resource-constrained settings.
Figure 3. Photo opportunity during the opening ceremony (A), ASP Team Meeting (B), hands-on workshop (C), panel discussion (D), clinical laboratory tour (E), pharmacy visit (F), pharmacist-led ward rounds (G), case discussion (H), lecture session (I), photo opportunity after the on-site inspection (J).
亞太地區抗生素管理師資培訓計畫
王如立1、鄭鈞文2、吳丁樹2、邱政洵3、蕭旋玲1,4
1林口長庚紀念醫院藥劑部
2林口長庚紀念醫院感染科
3林口長庚紀念醫院分子感染症醫學研究中心
4長庚大學呼吸治療學系
摘要
林口長庚紀念醫院於2018年發展並實施了一項為期一年的亞太地區抗生素管理種子師資培訓計畫,來自菲律賓和越南數家醫院的專家學者與醫療人員參與了此項計畫。此培訓計畫目的在為參與者提供建立和/或改善抗生素使用所必需的專業知識、領導能力與執行策略。此計畫組成包括培訓前的視訊電話會議、在林口長庚紀念醫院進行為期一周的跨領域討論會及臨床見習,以及活動結束後,培訓後的視訊電話會議及指導師資前往國外進行現場參訪。本文旨在分享本院執行此培訓計畫之事前準備及執行之經驗,並討論了藥師參與此類活動之重要性。
參考資料:
1. Wang CH, Hsieh YH, Powers ZM, et al. Defeating Antibiotic-Resistant Bacteria: Exploring Alternative Therapies for a Post-Antibiotic Era. Int J Mol Sci. 2020;21(3):1061. doi:10.3390/ijms21031061
2. Zhen X, Lundborg CS, Sun X, et al. Economic burden of antibiotic resistance in ESKAPE organisms: a systematic review. Antimicrob Resist Infect Control. 2019;8:137. doi:10.1186/s13756-019-0590-7
3. Center for Disease Control and Prevention. Antibiotic/Antimicrobial Resistance. https://www.cdc.gov/drugresistance/about.html (Accessed on June 07, 2020).
4. Chan YY, Lin TY, Huang CT, et al. Implementation and outcomes of a hospital-wide computerised antimicrobial stewardship programme in a large medical centre in Taiwan. Int J Antimicrob Agents. 2011;38(6):486-492. doi:10.1016/j.ijantimicag.2011.08.011
5. World Health Organization. One Health. https://www.who.int/news-room/q-a-detail/one-health (Accessed on June 07, 2020).
6. Goff DA, Kullar R, Goldstein EJC, et al. A global call from five countries to collaborate in antibiotic stewardship: united we succeed, divided we might fail. Lancet Infect Dis. 2017;17(2):e56-e63. doi:10.1016/S1473-3099(16)30386-3
7. Center for Disease Control and Prevention. Core Elements of Hospital Antibiotic Stewardship Programs. https://www.cdc.gov/antibiotic-use/core-elements/hospital.html (Accessed on June 07, 2020).
8. Waters CD. Pharmacist-driven antimicrobial stewardship program in an institution without infectious diseases physician support. Am J Health Syst Pharm. 2015;72(6):466-468. doi:10.2146/ajhp140381
9. Goff DA, Karam GH, Haines ST. Impact of a national antimicrobial stewardship mentoring program: Insights and lessons learned. Am J Health Syst Pharm. 2017;74(4):224-231. doi:10.2146/ajhp160379
10. Park S, Kang JE, Choi HJ, et al. Antimicrobial Stewardship Programs in Community Health Systems Perceived by Physicians and Pharmacists: A Qualitative Study with Gap Analysis. Antibiotics (Basel). 2019;8(4):252. doi:10.3390/antibiotics8040252
11. Cunha CB. Antimicrobial Stewardship Programs: Principles and Practice. Med Clin North Am. 2018;102(5):797-803. doi:10.1016/j.mcna.2018.04.003
通訊作者:蕭旋玲/通訊地址:桃園市333龜山區復興街5號 林口長庚紀念醫院 臨床藥學科
服務單位:林口長庚紀念醫院藥劑部/聯絡電話:(O) 03-3281200 ext 3730